ePCS/eKIS:
ePCS/eKIS is a significant development which allows GPs and District Nurses to record information on the palliative and end of life needs of their patients onto their GP software system, and for this to be available to those providing care in the Out of Hours period. For more information see Module 7 or access the Scottish Government website.
DNACPR:
Clinicians working across NHS Scotland are able to make decisions regarding the appropriateness of Cardiopulmonary Resuscitation (CPR), issuing a DNACPR instruction if considered clinically appropriate.
The responsibility for deciding if resuscitation is in the patient’s best interests lies with the patient’s lead clinician and any decision made regarding CPR will be based on a full consideration of the patient’s case.
Scottish Government have introduced a policy intended to prevent inappropriate, futile and/or unwanted attempts at CPR which may cause significant distress to patients and families as a death with an inappropriate CPR attempt may be undignified and traumatic. When a patient dies at home or in a care home an inappropriate CPR attempt is likely also to involve the Scottish Ambulance Service paramedics and even the police, which can add greatly to the distress for the families and be upsetting for all those involved. This policy is intended as a positive step to help a person’s wishes to be followed at the end of life irrespective of whether they are being cared for in hospital, hospice, care home or in their own homes. There is much confusion and uncertainty about CPR and the process of making advance decisions that CPR should not be attempted. Variations in local policies can cause misunderstandings and lead to distressing incidents for patients, families and staff. Increased movement of patients and staff between different care settings in Scotland makes a single integrated and consistent approach to this complex and crucial area a necessity. Access for further info:
NHS Scotland: Do Not Attempt Cardiopulmonary Resuscitation [PDF]
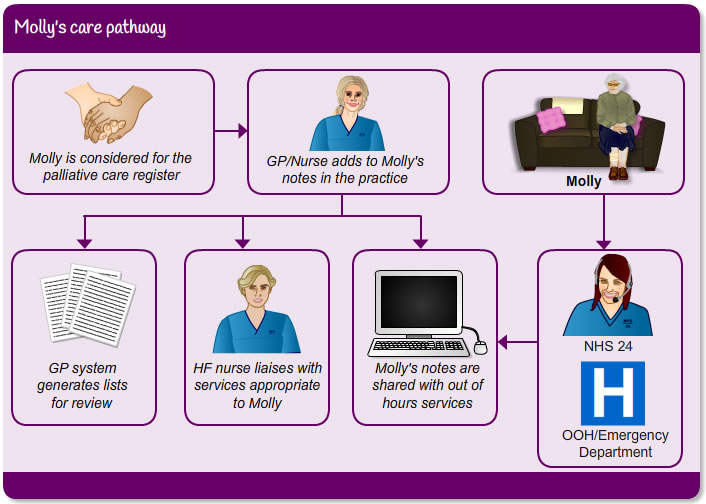
Adequate communication is vital when considering integrated palliative care approach to care for Molly´s wishes. Alongside these, DNACPR should be considered so the person´s competency can be assessed to make make the best decisions for the future.
- Molly is considered for the palliative care register
- GP/nurse adds to Molly’s notes in the practice
- GP system generates lists for review
- HF nurse liaises with services appropriate for Molly
- Molly’s notes are shared with out-of-hours services, so that if Molly contacts NHS24 or OOH/Emergency department, they will be able to get up to speed with her up-to-date medical history
Pulse point
All these services will vary in your areas but are vital support for Molly in this period of her heart failure management.
Think about what other support would be available for Molly in the community in the area where you work. Keep in mind that for someone living with a long term palliative condition that social support can often be just as important as medical intervention.
Continuity of care is vital to be able to detect subtle changes in a patient´s condition. Where possible an appropriate member of the multi-disciplinary team should be identified to co-ordinate and implement advance care planning with the patient and carer.
“A joined up, consistent approach improves quality of life for the patient and family/carer”
Ref: NHS QIS 2010 [.pdf]
Page last reviewed: 28 Jul 2020


