Implementing Bill’s care wishes requires effective verbal and written communication which should be shared with all members of the multi-disciplinary team. The professional who knows Bill well and who has a good relationship with is best placed to co-ordinate the sharing of information.
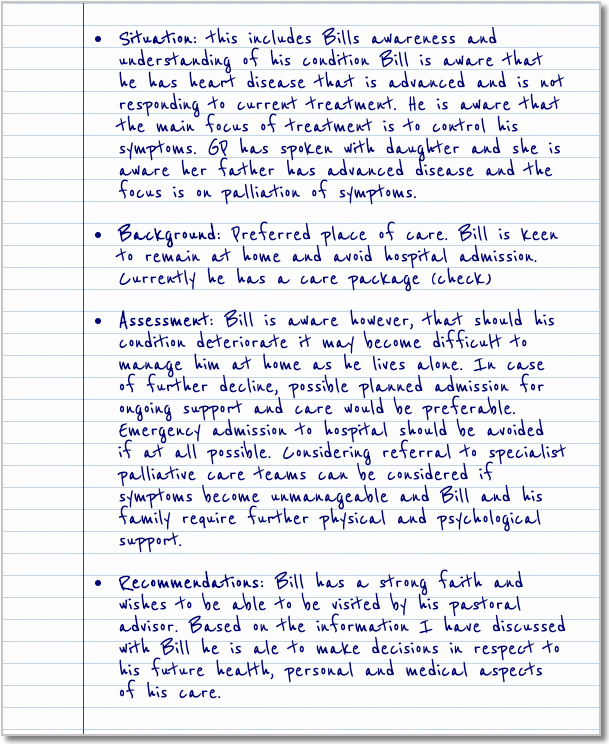
- Situation: this includes Bills awareness and understanding of his condition Bill is aware that he has heart disease that is advanced and is not responding to current treatment. He is aware that the main focus of treatment is to control his symptoms. GP has spoken with daughter and she is aware her father has advanced disease and the focus is on palliation of symptoms.
- Background: Preferred place of care. Bill is keen to remain at home and avoid hospital admission. Currently he has a care package (check)
- Assessment: Bill is aware however, that should his condition deteriorate it may become difficult to manage him at home as he lives alone. In case of further decline, possible planned admission for ongoing support and care would be preferable. Emergency admission to hospital should be avoided if at all possible. Considering referral to specialist palliative care teams can be considered if symptoms become unmanageable and Bill and his family require further physical and psychological support.
- Recommendations: Bill has a strong faith and wishes to be able to be visited by his pastoral advisor. Based on the information I have discussed with Bill he is ale to make decisions in respect to his future health, personal and medical aspects of his care.
Pulse point
Anticipatory Care Planning is not a one of event and should be regarded as a process involving several discussions.
This is an example of information gathered for a care plan. Formats will differ across areas and patients but the information included can be universally accepted. For further information regarding care planning access:
Living and Dying Well
Recognised that the key to providing appropriate palliative and end of life care is first of all to identify those likely to benefit from it, and then to initiate a cyclical process of assessment and review to determine the ongoing palliative care needs of patients and their families. This may be at any time from the point of diagnosis, at the point of actual or anticipated deterioration, or on presentation of difficult or complex symptoms. In each of these cases, the consistent use of appropriate assessment tools is essential. To ensure a coherent national approach to this issue, SLWG 3 was established to develop recommendations regarding:
- assessment tools for early identification of patients who may need palliative care
- assessment tools to identify patients with increasing palliative care needs
- assessment tools for symptoms.
Page last reviewed: 29 Jul 2020


