Definition of the test
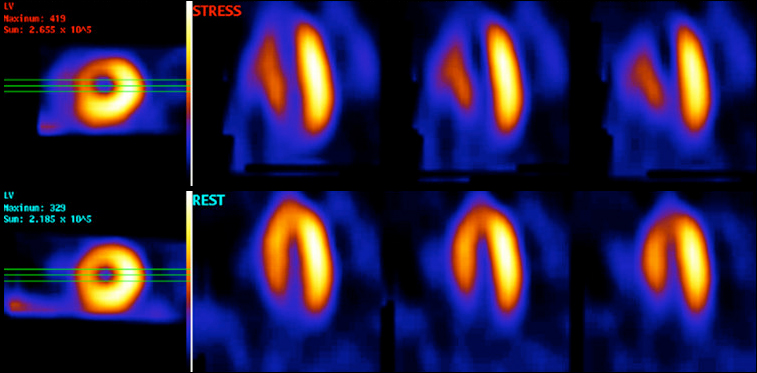
A myocardial perfusion scan (also known as myocardial perfusion scintigraphy) is a non-invasive nuclear medicine imaging test which uses a small amount of a radioactive tracer to investigate the blood supply to the heart. It is a functional test which can detect any difference in blood flow to the heart muscle at rest and during stress (which may be exercise stress or pharmacological stress). It can also be used to assess the extent of damage to the heart after a heart attack. It does not look at the coronary arteries themselves; rather it looks at the blood supply to the heart muscle, from which inferences can be made about the arteries.
The requirements for a MPS include a radioactive tracer, a stressor and a gamma camera. The radioactive tracer (which may be technetium, thallium or others) emits radioactivity in the form of gamma rays. Once it is injected into a vein, it travels in the bloodstream and is taken up by heart muscle. Areas of the heart that have a good blood supply will take up a large amount of tracer, whereas areas of the heart with a poor blood supply will take up a smaller amount of tracer. Therefore, areas of heart muscle with a good supply will emit more gamma rays than areas with a poor blood supply.
Radiation emitted by the tracer is detected by a gamma camera, and converted into an image on a computer.
What it involves
There are a number of different protocols for performing a MPS, which vary from hospital to hospital. Many centres utilise a two part scan, whereas some perform the whole scan on one visit. The test will involve a ‘stress’ part and a ‘rest’ part, to allow comparison of blood flow during stress and rest.
If the planned test involves pharmacological stress, patients will have been asked to withhold/avoid certain medications or drinks containing caffeine for a day or two prior to the appointment. If this is required, the patient appointment letter will usually contain this information.
On arrival at the nuclear medicine department, the patient will be prepared and consented as for any invasive procedure. See ‘Additional Information’ for a patient video on this test.
During the stress part of the test, the heart is made to work harder either with gentle exercise on a treadmill or bicycle, or alternatively with infusion of a drug. Some common drugs that might be used are those which make the heart beat stronger and faster, such as dobutamine, or those which vasodilate (open up) the arteries and increase blood flow to the heart, eg adenosine or dipyridamole. Adenosine and dipyridamole are generally not used in patients with reversible airways disease such as asthma, as they can cause bronchoconstriction and breathlessness. Once the stressor has been given, the radioactive tracer will be injected and the patient will be asked to lie in the scanner to allow the gamma camera to detect the emitted gamma rays. Patients are usually required to place their arms above their head whilst the scan is being performed, and lie as still as possible. The scan can take up to 30 minutes.
The stress scan images will generally be reviewed by a nuclear medicine consultant, radiologist or cardiologist and a decision made as to whether the patient requires to return for a ‘rest’ study. This will depend upon the reason for the test and whether there are any abnormalities on the stress study. If the patient requires to return for a rest study, this will involve an injection of the radioactive tracer followed by a scan – this part is usually much quicker, as there is no need for exercise or pharmacological stress.
Which patients might a MPS be used on and why?
MPS is used to identify whether there is a problem with the blood flow to the heart muscle, or to assess how much damage has been done to the heart after a myocardial infarction. It is therefore of use in patients:
- With chest pain, to help diagnose or rule out angina
- With an abnormal coronary angiogram, to help identify which narrowed artery is likely to be the culprit for angina (and therefore which artery should be treated).
- With impaired left ventricular function on echo – to assess whether the areas of the heart which are not contracting well are still viable (and worthy of restoring the blood flow to) or not.
How is MPS used to diagnose a cardiac condition?
When assessing blood flow to the heart in a myocardial perfusion scan, we look at whether there is a difference in regional myocardial blood flow at rest and following stress. There are three main possibilities:
- If the blood supply at rest is normal, but the blood supply following stress is reduced, this indicates that there is reversible myocardial ischaemia which is likely to be due to a narrowing in a coronary artery. This is called a reversible perfusion defect. By comparing the tracer uptake in the various different areas of the heart (the coronary artery territories) we can work out which artery or arteries are likely to have a narrowing. Such patients might go on to have an invasive coronary angiogram to identify the narrowings and potentially treat them.
- If blood supply at rest is the same as blood supply following stress, it is unlikely that there is significant obstructive coronary artery disease. This is a normal myocardial perfusion scan. For patients with chest pain, a normal myocardial perfusion scan is associated with a rate of MI or cardiac death of less than 1% per year. It is therefore a good ‘rule out’ test for significant obstructive coronary disease.
- If blood supply at rest is abnormal but is similar to the blood supply following stress, this suggests that there has been previous myocardial infarction in the area of reduced blood supply. This is called a fixed perfusion defect. Such fixed defects can represent either viable or non-viable myocardium – the former might recover function with revascularisation whereas the latter will not.
The stress and rest images will be reviewed by a nuclear medicine consultant/cardiologist/radiologist and a report generated for the referring doctor. Patients will not normally receive the result on the day of the scan.
| Benefits | Risks |
|---|---|
|
|
Page last reviewed: 30 Jul 2020


