Archies’ oxygen saturation should be maintained between 94-98%-
In cases of acute hypoxaemia, treatment may be started with nasal cannulae. The flow rate should be adjusted to achieve a saturation of 94–98%. BTS guideline for oxygen use in healthcare and emergency settings (2017)
Information on oxygen therapy as related to stroke: The British Thoracic Society (BTS) guideline for oxygen use in adults in healthcare and emergency settings (2017) recommend- high concentrations of oxygen should be avoided in patients with stroke, unless required to maintain normal oxygen saturation. Aim at an oxygen saturation of 94–98% or 88–92% if the patient is at risk of hypercapnic respiratory failure.
Good practice points regarding stroke management-
✓ Oxygen saturation should be monitored at least every 4 hours throughout the day and night in patients with acute stroke and all episodes of hypoxaemia treated.
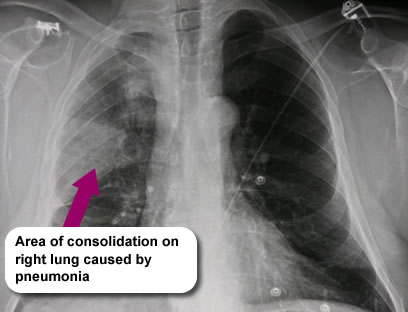
✓ Patients with hypoxaemia post-stroke require medical review to establish and treat the cause.
✓ Oxygen should only be given once the airway has been cleared and at the lowest concentration necessary to achieve an oxygen saturation of 94–98% or 88–92% if the patient is at risk of hypercapnic respiratory failure.
✓ Oxygen should be given via nasal cannulae, unless there are clear indications for a different oxygen delivery system.
✓ Patients with stroke and cardiorespiratory comorbidities should be positioned as upright as possible, in a chair if possible.
✓ Patients with a reduced level of consciousness after stroke should be nursed in the recovery position with the paralysed side lowest. These good practice points in stroke are taken from BTS guideline for oxygen use in healthcare and emergency settings (2017).
How do you give oxygen accurately?
The amount of oxygen on the flow meter (in litres/min) on the wall should always match the coloured delivery device attached to the mask (measured in % oxygen delivered to the patient).