On returning home, Trevor continued to have occasional emotional outbursts but these are less frequent and less distressing for him. He has found that socially the emotional lability has not been as problematic as he had anticipated. Trevor remains on low-dose antidepressants which he feels are helpful.
Following the education and support the family received in the rehabilitation unit on emotional lability they were able to continue to use the strategies they had been taught. These proved to be extremely helpful and beneficial to Trevor, his family and friends.
Although Trevor’s functional abilities continued to improve his dense hemiplegia and mild cognitive impairment meant that he was unable to return to his engineering business in his previous capacity. His business partner bought over Trevor’s share of the business and was able to find a role which suited Trevor.
- Trevor has a good response to combined treatment
- Outbursts are still present but less frequent and less severe in nature
- Trevor feels better able to cope with them due to his increased understanding of why he has them. However, he finds some of the distraction techniques difficult to put in place and needs prompting to do so
- He reports benefitting from having the time and space to speak with John about how he is feeling about his stroke
- His family feel they have a better understanding of his crying and are better able to deal with his outbursts and support Trevor with them
- His son is now visiting on a more regular basis although he is still struggling to cope with the changes in his dad. The Social Worker has discussed this with Tom and is looking into referring Tom to a local young carers’ group for further support
- Staff continue to evaluate Trevor’s progress and discuss this at the MDT meetings
A review of Trevor’s Patient Health Questionnaire (PHQ-9) showed that there had been an improvement: Patient Health Questionnaire (PHQ-9) [2] [.pdf, 225KB]
See Additional Information box for more information on the PHQ-9.
Trevor tells the medical and nursing staff on the ward round that he feels more comfortable due to discussions with staff and his use of coping strategies. He doesn’t feel so embarrassed now that he knows that emotional lability is common following a stroke and that it is not about him not coping. Nurse Jones completes another PHQ-9 form to monitor changes in Trevor’s condition.
However, Trevor feels that his emotional outbursts are still somewhat disruptive to his rehabilitation and he is worried how these outbursts may affect him when he goes home. He is particularly worried about crying in public and how people who don’t know him or know about emotional lability may react.
Trevor feels that a diary would be useful to allow him to record how he is feeling. He can then explore the coping strategies that help him.
Click through the diary pages using the < and > buttons on the images.
Following a discussion with his doctor, concerning the possible side-effects, Trevor agrees to try a low dose of anti-depressants. Both the frequency and intensity of emotional lability is thought to be reduced by anti-depressants and often these can be effective within one week.
However anti-depressant treatment is usually only considered if the emotional lability is disrupting the patient’s rehabilitation programme (SIGN 118 2010, RCP 2016).
While Trevor is having this medication it would be important to ensure that his personal diary is maintained and staff observations continue to be noted, to monitor for any improvements in Trevor’s symptoms. Treatment with anti-depressants in emotional lability is not successful in every case.
Nurse Jones pages John with the referral explaining that Trevor is suffering from emotional lability which is causing him
- to cry uncontrollably
- distress because it is completely out of character and his family are finding it very difficult to cope with his crying
- frustration that these outbursts are interrupting his rehabilitation
In addition to the immediate physical symptom control of Trevor’s emotional lability, an holistic approach to healthcare requires emotional and spiritual support which recognises and addresses the anxieties, fears and questions that routinely arise when health breaks down. Ward staff, doctors and health care professionals will be aware of the mood swings and anxieties patients and relatives express and, as time allows, would try to address these.
Nurse Jones suggests to Trevor that he might appreciate having a conversation with the chaplain who routinely visits in the ward. John (chaplain) would have time to sit for a while if Trevor wanted to talk over how he is feeling about all that had happened. Trevor agrees, saying he thinks ‘that wouldn’t be a bad idea’.
Having identified a desire on Trevor’s part to talk in more depth with the chaplain, if a relationship of trust develops, it would be appropriate for that support to continue.
Good emotional and spiritual care happens when specific needs are perceived and support offered, on the patient’s terms. Such care is integral to the well-being of the patient and immediate carers. Everyone involved with Trevor and his care may contribute to this kind of support. However, people often value the opportunity to speak to someone who is not directly involved in their medical care.
An integral part of the team’s role is to provide education and information provision to patients and their families/carers.
The doctor has explained to Trevor that he is experiencing emotional lability, Nurse Jones also talks about coping strategies, medication and ongoing emotional support. She provides them with the following publications and encourages the family to raise any worries or concerns they might have at any time.
Good practice points for providing information: (SIGN 118)
- Information should be made available to patients and carers routinely, in a variety of formats
- Information should be tailored to the information needs of individual patients and carers
- Check patient and carer understanding of the information provided to ensure clarity
- Information needs should be monitored as these needs can change over time
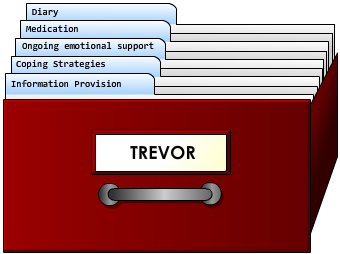
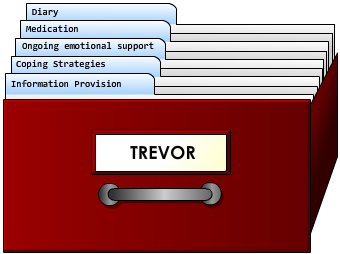
Now that Trevor has been diagnosed with emotional lability an appropriate treatment plan can be developed.
Check his treatment folder for further information on how the multidisciplinary team are supporting Trevor.