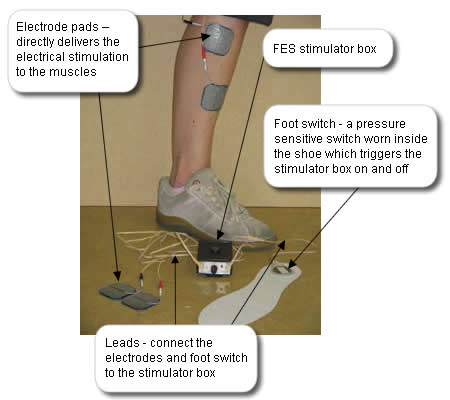
Alan’s physiotherapist is trained in the application of an alternative orthotic device for managing his dropped foot, Functional Electrical Stimulation (FES). She feels that this device may benefit Alan so she discusses it in detail with him, provides written information and gives him time to consider if he wishes to try it.
An FES Device
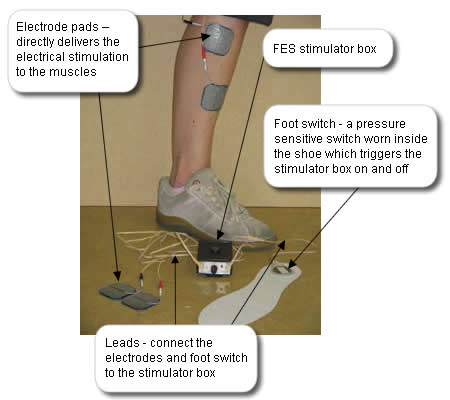
Watch the video below to see a stroke patient who presents with a dropped foot walking. Then watch the same gentleman walking but this time using an FES device to correct his dropped foot.
Duration: 1 minute 1 second (no audio)
The FES Device shown is Odstock Dropped Foot Stimulator (ODFS) from Odstock Medical Limited Salisbury. Other and newer FES devices are available .
Definition:
FES is a means of producing contractions in muscles paralysed due to central nervous system lesions (eg stroke) by means of electrical stimulation to the peripheral nerve (the nerves that are out with the brain and spinal cord). This stimulation is used to produce a functional movement e.g. lifting the affected foot during the swing phase of walking. Stimulation can be applied via surface-applied or implanted electrodes.
Impact of FES:
FES potentially has a therapeutic effect. This being the effect seen when the stimulator is switched off. By its mode of action, namely stimulating muscle, FES may encourage motor recovery.
Similarly to an AFO it also has an orthotic effect that being the effect seen while the stimulator is switched on.
Contraindications:
Exposed orthopaedic metal work on the lower limb; tumour in the area of stimulation; uncontrolled epilepsy; lower motor neurone conditions (conditions that have caused damage to the peripheral nerve)
Cautions:
Marked spasticity, poor skin condition; marked oedema (swelling); pregnancy; pacemakers; fixed ankle contracture
Rationale:
Alan meets the inclusion criteria for FES. Additionally, as Alan has some motor activity at his ankle it is considered that FES may help the motor recovery of his ankle and forefoot muscles. Following his discussion with the physiotherapist Alan is keen to try it and is therefore set up and provided with FES.
References:
| Ankle Foot Orthosis (AFO) |
| Why use it? |
An AFO can be used to assist with a patient’s walking. It can be used to directly control the dropped foot during the swing phase of walking. An AFO can also have an impact on the standing phase of walking by directly improving the stability and alignment of the ankle and foot on the ground which in turn may have an impact on the hip, knee and trunk position. |
| When to consider an AFO? |
As soon as the patient is medically stable consideration can be given to the provision of an AFO. |
| Cautions |
Poor skin condition, marked and fluctuating oedema (swelling), sensory loss, poor circulation, severe spasticity and marked contracture. |
| Rationale |
Alan has a dropped foot which causes his foot to catch when he swings his leg through during walking. Additionally when he stands on his leg his knee flicks back. The provision of a custom made AFO will help him swing his leg through during walking and indirectly reduce the flick of his knee into extension on standing. It is hoped that this will improve his gait pattern, independence and balance and reduce the effort of walking and potential for trauma to his knee joint. |
Reference: NHS Quality Improvement Scotland: Use of ankle-foot orthoses following stroke – Best Practice Statement

Q. What is an AFO and what does it do?
Ankle Foot Orthosis (AFO): An AFO is a device worn on the lower part of the leg to provide direct control of motion and alignment of the ankle and foot.
Answer yes or no to the following statements about the Ankle Foot Orthosis (AFO).
Q. Alan is to commence walking on the ward. What needs to be considered now? Select the crosses next to the labels to find out more.
He starts walking with supervision of a nurse to and from meals and requires a stick and an AFO. Alan is aware of the technique to use and the safety issues.
Alan is keen to walk on the ward. The key worker takes Alan’s request to the MDT meeting.
Go through the slides to see each of the team members and view their discussion.
Alan can stand unaided but tends to lose his balance when reaching for objects and has active movement in his hip and knee but his leg is generally weak. He has flickers of movement at his ankle but is unable to pull his foot up. When walking Alan presents with a dropped foot. This means that he can’t lift his foot clear of the ground when swinging his leg through and is at risk of falling. Additionally when standing on his leg his knee tends to flick back into hyperextension (sudden uncontrollable straightening of the knee beyond normal – see photograph below) which could cause long term damage to his knee joint. Alan has been provided with a custom made ankle foot orthosis (AFO) to help with these issues and is currently walking in therapy with the help of a therapist.
Photograph showing a hyperextended knee

Alan approaches you and says that he wishes to walk on the ward. How should you manage this?
Alan has had Botulinum Toxin to his finger and wrist flexors and stretches and exercises to improve the motor control. This has helped his hand and has improved the functional use of his arm. He can now clean his hand and has flickers of active movement at his wrist and fingers. Following education in stretches and application of the splint, Alan feels that he is competent to apply it. He is happy with the management of his hand and is less distressed about the appearance of his hand.
Why would splinting be used?
- May reduce pain (by providing support to joints)

- May reduce deterioration from spasticity
- May prevent contracture
- May increase range of movement
- May block unwanted movement
- May improve function
- May improve hand hygiene
Caution: Hand splinting alone will not improve upper limb function or reduce tone. It is a valuable adjunct to other management interventions such as physiotherapy, spasticity management etc. It is therefore important that there is careful consideration for the rationale for selecting this intervention.
Alan has been provided with a custom made hand splint by the therapist. Splint application can be effective if there is good team working. Drag the possible solutions to match the potential issues that may occur.
Alan’s spasticity management goals are to:
- Improve his hand hygiene
- Improve his body image
- Increase the functional use of his arm
The main aim is to optimise the outcome of his upper limb rehabilitation
As part of his spasticity management Alan attends a spasticity management clinic for assessment and treatment options. As as result of this assessment he has had Botulinum Toxin injections into his wrist and finger flexors. In order to maximise the benefit of this he now needs to follow an appropriate management plan including:
- Stretches (to maintain and increase muscle and soft tissue length)
- Splinting (to provide a good position and optimise the muscle and soft tissue length)
- Exercises (to facilitate activity and strength in the opposing muscle groups)
- Patient education (of stretches, exercises, splint application and to encourage long term self management)
- Upper limb functional tasks (to encourage self practice and overall upper limb function and activity)
For a description of what a spasticity clinic is see additional information.
Link: Spasticity in adults: management using botulinum toxin National guidelines (2nd edition).RCP March 2018 (PDF).