Following clinical assessment Mrs McGinty was found not to have a DVT. However, because of the risks associated with her calf pain, chronic conditions, age and immobility possible DVT had to be considered and screened for using the Wells Score Risk Assessment Tool. Patient with either calf pain, or unilateral ankle, calf or leg swelling needs to have DVT excluded. Similarly, the development of sudden breathlessness, low oxygen saturations, haemoptysis or a new cough requires clinical staff to consider and screen for a Pulmonary Embolism.
To learn more about DVT and PE prevention visit STARs Advancing Module 17: Reducing the risk of venous thromboembolism.
Mrs McGinty is recovering well from her chest infection but complains of a throbbing pain in her calf. Deep vein thrombosis (DVT) of the legs is common in patients with a recent stroke, particularly in older patients with severe hemiplegia who are immobile.
Owing to her communication problems Mrs McGinty is finding it difficult to describe her symptoms to the nurse but is able to indicate that there is something wrong with her calf. On observation the nurse notes that Mrs McGinty’s calf is red and is concerned that she may have developed DVT.
- Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in the leg/s. Deep vein thrombosis can cause leg pain or swelling but DVT can also occur with no symptoms. DVT is considered a serious condition. Blood clots in the vein/s can break loose, travel through the bloodstream and get stuck in the lungs, blocking blood flow (pulmonary embolism). However, pulmonary embolism can occur with no evidence of DVT. This can cause symptoms such as: sudden shortness of breath, chest pain or discomfort that gets worse with deep breaths or coughing. The person may have rapid breathing, feel lightheaded, dizzy, or faint.
- Mrs McGinty was commenced on Intermittent Pneumatic Compression (IPC) therapy when she was initially admitted to the stroke unit. IPC is used to help prevent blood clots in the deep veins of the legs. IPC therapy is recommended for use in immobile acute stroke patients and should be commenced on admission to the stroke ward in accordance to the Scottish Stroke Care Audit (SSCA) guidance & Scottish Stroke Improvement Programme (SSIP) plan, priorities and actions.
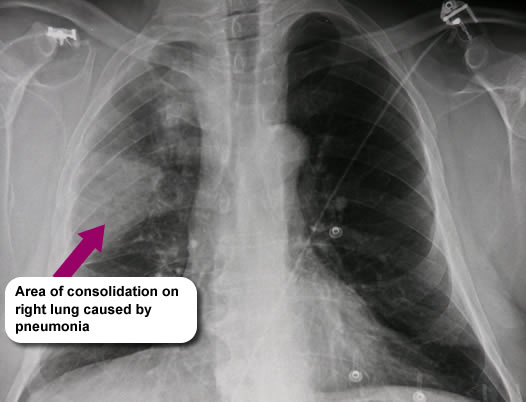
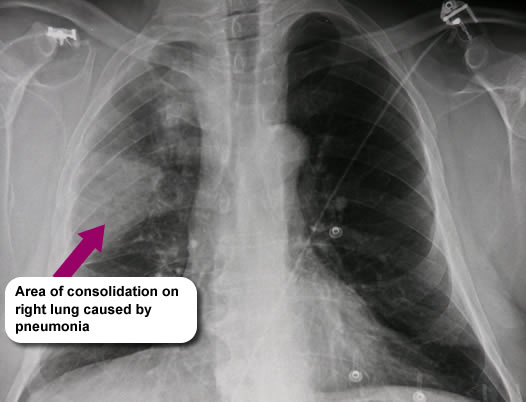
Twenty-four hours later, whilst carrying out a routine set of observations the nurse noticed that Mrs McGinty had a raised temperature of 38.1°C and that she was sounding chesty. A chest X-ray was carried out and she was diagnosed with a chest infection.
Mrs McGinty was managed according to local protocols – her pressure ulcer did not progress and subsequently healed.
It is essential that you identify patients who may be at risk of developing pressure ulcers and take the appropriate preventative measures. Patients who present with existing pressure ulcers should receive appropriate treatment and must be closely monitored.
The most important way to prevent ulcers is to relieve the pressure on the tissues for long enough, and at frequent enough intervals, to allow the tissues to receive an adequate blood supply (Warlow et al 2019).
| Prevention of pressure ulcers |
| This can be achieved by: |
- Regular turning/positioning of the patient
- Regularly changing the patient’s situation e.g. time spent in bed/time spent in chair
- Use of appropriate continence products
- Use of appropriate skin cleansing, moisturisers and barrier products
- Utilise passive and active pressure relieving mattresses and cushions
- Passive systems include: padded mattresses, polystyrene bead system, foam mattresses, roho cushions, gel pads
- Active systems include: ripple mattresses and cushions, low air loss systems and more sophisticated forms of specialist equipment
|
| Treatment of pressure ulcers |
| For those with established pressure ulcers, pressure relief appears to be the most important factor in promoting healing which can be achieved by using the methods/equipment as per table above. Additionally you should consider: |
- Optimising the patient’s general condition e.g. good diet, adequate hydration
- Analgesia – this should be adequate to prevent patient distress and the development of spasticity
- Antibiotics – if local/systemic infection present
- Use of appropriate dressings and products
- Debridement – necrotic tissue should be removed
- Skin grafting – to achieve skin coverage
- Electrotherapy to promote healing
|
Reference:
- Warlow’s Stroke: Practical Management, 4th Edition (2019) Graeme J. Hankey (Editor), Malcolm Macleod (Editor), Philip B. Gorelick (Editor), Christopher Chen (Editor), Fan Z. Caprio (Editor), Heinrich Mattle (Editor).
Further reading:
Prevention and Management of Pressure Ulcers (2020) available at: Healthcare Improvement Scotland.
Tubaishat, A, Papanikolaou, P, Anthony, D, Habiballah, L (2017). Pressure ulcers prevalence in the acute care setting: a systematic review. Clinical Nursing Research, 27 (10), pg 1-28.
NB: You should check your local area for protocols and guidelines.
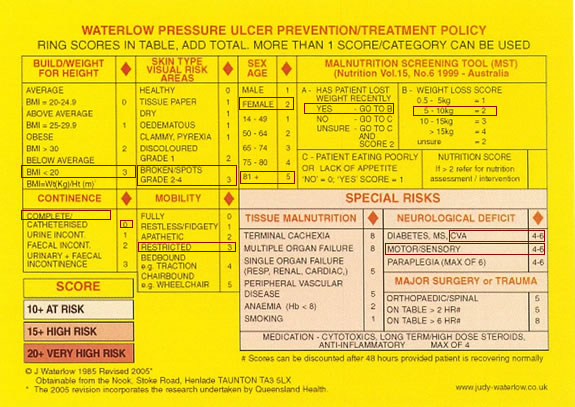
Mrs McGinty’s score is 26 (Very High Risk category). With this high level of risk Mrs McGinty would be managed according to local ward protocols but it is likely that she would require specialist pressure relieving equipment.
Healthcare Improvement Scotland (HIS) link to: Pressure Area Risk Assessment Warlow
Reference: Warlow’s Stroke: Practical Management, 4th Edition (2019) Graeme J. Hankey (Editor), Malcolm Macleod (Editor), Philip B. Gorelick (Editor), Christopher Chen (Editor), Fan Z. Caprio (Editor), Heinrich Mattle (Editor)
For further information on risk assessment visit: HIS: Risk Assessment
For information on grading pressure ulcers visit: HIS: Pressure ulcer grading.
For information on wound assessment visit: HIS: Wound assessment.
On admission to the ward all stroke patients should be routinely assessed to determine whether they have developed or are at risk of developing pressure ulcers. Those found to be at risk should have on-going monitoring. The Waterlow Scale is one of many clinical scoring systems developed to indicate an individual patient’s risk.
The nurse on the stroke unit has calculated Mrs McGinty’s score using the Waterlow Scale below:
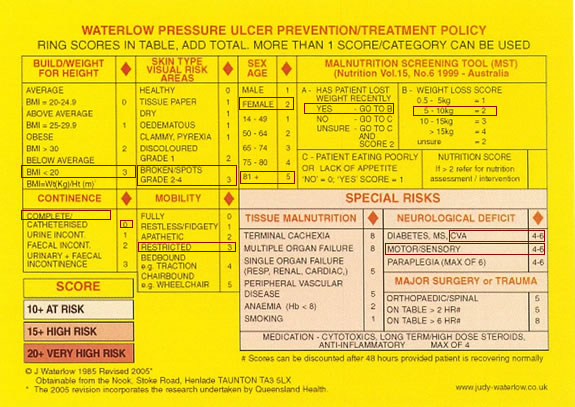
Mrs McGinty is 84 years old. Her daughter has reported that she has been eating poorly since her previous stroke and that she has lost approximately 7.5kg in weight resulting in a BMI score of 17.2. On admission to the stroke unit she had a partial thickness skin break on her sacrum. She is continent but has restricted mobility due a right sided hemiplegia.
Scottish Adaptation of the European Pressure Ulcer Advisory Panel (EPUAP) Pressure Ulcer Classification Tool: Grading Tool