Category: Advancing Modules
About pressure ulcers
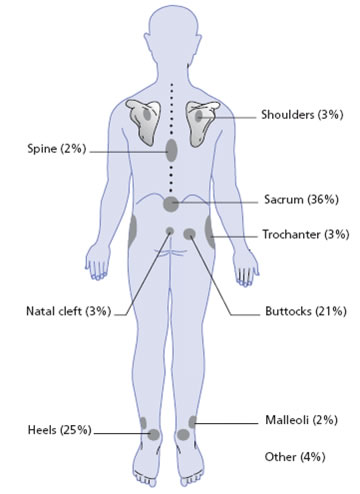
Pressure ulcers occur when local pressure on skin and subcutaneous tissues exceeds the capillary opening pressure for long enough to cause ischaemia. In addition, friction may cause blistering and tears in the skin. Pressure ulcers usually occur over weight-bearing bony prominences (see drawing below). Ulcers occur in patients who are immobile and unable to redistribute their own weight when lying or sitting.
See left for the anatomical distribution of established pressure sores, based on data from a cross-sectional UK study of pressure sores in patients being nursed on the Pegasus Airwave System.
Reference: Warlow’s Stroke: Practical Management, 4th Edition (2019) Graeme J. Hankey (Editor), Malcolm Macleod (Editor), Philip B. Gorelick (Editor), Christopher Chen (Editor), Fan Z. Caprio (Editor), Heinrich Mattle (Editor)
Admission
It is noted by the staff in A&E that Mrs McGinty has developed a partial-thickness skin break on her sacrum. Her daughter provides some further background information explaining that she had found her Mum this morning on the floor having last seen her on Friday evening. She doesn’t know how long she had been lying there but judging by her position and general state she thinks it may have been for some time. She also reports that her Mum had been incontinent and it looked like she had tried to drag herself around the room to get help.
On admission to the stroke unit the nurses further assess and consider how best to manage her sacral partial-thickness skin break.
The presenting features of a patient with PACS
Patients may present with one or more of the following:
- New, higher cerebral dysfunction (such as aphasia, inattention, dyspraxia, agnosia)
- Homonymous visuospatial field deficit
- Limited weakness or sensory loss involving the face, arm or leg
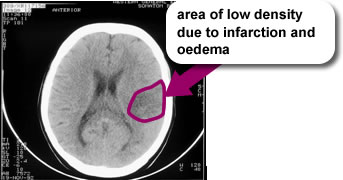
This CT scan shows a small left hemisphere cortical infarct which might result in a PACI clinical syndrome
Predicted outcomes at 30 days post PACI:
- 5% of patients dead
- 40% of patients dependent
- 55% of patients independent
What is a Partial Anterior Circulation Syndrome?
The Oxford Community Stroke Project (OCSP) classification describes the clinical presentation of stroke and is useful in clinical practice and research.
Using this system, stroke patients are first classified as TACS (where ‘S’ denotes Syndrome), PACS, POCS or LACS until cerebral imaging allows the differentiation between infarction and haemorrhage.
Infarcts were subdivided according to clinical presentations when their symptoms were maximal. Stroke subtypes were classified as follows:
| Stroke Subtype | Percentage (%) of infarcts |
|---|---|
| Total Anterior Circulation Infarcts (TACI) | 17% |
| Partial Anterior Circulation Infarcts (PACI) | 34% |
| Posterior Circulation Infarcts (POCI) | 24% |
| Lacunar Infarcts (LACI) | 25% |
Her story
Mrs McGinty’s daughter found her lying on the floor. She called 999 for an ambulance to take her to hospital. Where Mrs McGinty presented with a mild hemiplegia affecting her right arm and leg, aphasia and apraxia, consistent with a left hemisphere Partial Anterior Circulation Syndrome (PACS).
Case 2: Mrs McGinty
 Mrs McGinty is an 84-year old woman who lives alone in her own home. She has a daughter who lives nearby and she has one cat.
Mrs McGinty is an 84-year old woman who lives alone in her own home. She has a daughter who lives nearby and she has one cat.
She is an ex-smoker and claims to be a social drinker. She has chronic obstructive pulmonary disease (COPD), diabetes and moderate hypertension.
She had a minor stroke 6 months ago which affected her right side, was independent with her personal care and had some support from her daughter with domestic tasks. She is 1.56m tall and weighs 42kg.
Key Messages
The following Word Search summarises the main themes of intervention and prevention, see if you can find them.
Outcome
![]() Three weeks later Mr McTavish has an appropriately fitted shoulder support, an effective analgesic prescription and no longer has shoulder pain which interferes with his ability to participate in rehabilitation.
Three weeks later Mr McTavish has an appropriately fitted shoulder support, an effective analgesic prescription and no longer has shoulder pain which interferes with his ability to participate in rehabilitation.
He can now transfer independently and is walking short distances with support.
Mr McTavish is in the process of discharge planning and, once home, he will continue with his stroke rehabilitation therapy in the community.
Careful handling of the upper limb
Patients with hemiplegia may not be able to move their limbs normally and they may also be unable to care for their limbs appropriately. As a result of this you may have to assist patients with varying degrees of paralysis to move their limbs during care and therapeutic activities. It is important that this is done carefully and within their normal, pain free range of movement so as to prevent damage. For further advices and support liaise with members of the multi disciplinary team (MDT).
These videos contain sound, please ensure that the computer you are using has sound enabled and speakers or headphones.
For more video footage showing correct moving and handling of patients visit Stroke4Carers, section on: Basic moving and handling for carers


