- This is repetitive voluntary contraction and relaxation of the pelvic floor muscles.
- Pelvic floor exercises have been successfully used since the 1940’s for the treatment of stress urinary incontinence and mixed urinary incontinence.
- An individual treatment programme of pelvic floor exercises is very effective in treating female patients and may be helpful for men following prostate surgery.
- Pelvic floor exercises should be carried out, ideally after digital assessment to identify strength and duration of the contraction of the pelvic floor. Assessment should also exclude prolapse and atrophic vaginitis.
- Pelvic floor exercises should involve maximum effort and include a sustained muscle contraction (6-10 seconds) followed by an equal period of full muscle relaxation. Two to three sets of 10 pelvic floor muscle exercises should be completed each day.
- Pelvic floor muscle exercises can be used in combination with a bladder training programme to assist with bladder rehabilitation.
- The use of the mid stream stop exercise is no longer recommended and should be avoided.
- There are a range of useful apps and YouTube videos available which may support patients doing pelvic floor exercises. Please note some apps may incur a small cost.
Category: Advancing Modules
Self monitoring
For people with mild to moderate bladder and bowel issues self-monitoring may be effective but it requires good cognitive function.
It involves lifestyle changes including:
- Fluid management to ensure daily intake of 1500 -2000mls.
- Avoiding constipation.
- Cutting down or eliminating caffeine.
- 3-4 hourly voiding, no longer intervals.
- Use of ‘the Knack’ to suppress urgency and brace the pelvic floor. ‘the Knack ‘ is a quick contraction of the pelvic floor. Several quick contractions can help the person to control urgency.
Bladder training
- A programme of bladder training has no side effects and does not preclude any other treatment. It is useful as a behavioural treatment particularly for older people who often experience side effects of medication
- Bladder training involves the person learning to resist the desire to go to the toilet
- It aims to stretch the bladder and reduce overactivity/ hypersensitivity
- Key point – Any person who engages with bladder training needs to be motivated and encouraged to follow the programme as initially it can be very difficult to defer the need to void. It is important that the patient’s motivation is sustained with good support throughout the process
- A training programme gradually increases the time between voids over a 6 week period. The person should comfortably reach 3-4 hourly voiding
- Bladder training should begin with individual written and verbal information
- A reasonable and realistic interval of scheduled voiding should be introduced. The person is then guided to defer toilet visits by 5 to 15 minutes each week
- Deep breathing, relaxation and mental distraction techniques are taught to help control urgency feelings
- At the start of the programme the person may experience increased episodes of leakage but this is to be expected and will improve as the programme continues
- Training is not carried out during the night. However if bladder training is successful it helps to improve night time frequency (nocturia)
- Some people with severe urgency find bladder training difficult. They may benefit from the addition of an antimuscarinic medication but there must not be any incomplete emptying (common after stroke) as the use of antimuscarinic medication may increase post-void urinary residuals.
Read the Consensus statement on bladder training and bowel training article.
Caffeine quiz
Daily intake of caffeine should not exceed? Select the correct answer.
Fluid Management
- Identify at the outset what the person is drinking , the volume and type of fluid.
- Review the fluid balance chart and bladder diary. This will allow a detailed account of toileting habits, bladder output and pattern of fluid intake.
- It is important that any person with bladder problems drinks 1.5 -2 litres each 24 hour period.
- Consider how other symptoms may affect timing of fluid intake e.g. nocturia.
- Also note signs of dehydration, dry mouth or complaints of constipation.
- Caffeine releases calcium from intra cellular stores in the smooth muscle of the gut. It can produce a hyper active bladder with symptoms of urgency.
- Caffeine also has a mild diuretic effect so changing fluid types may have a significant effect on bladder symptoms.
- Caffeine free fluids are recommended: Avoid tea, coffee, hot chocolate, Irn Bru™, Cola and energy drinks.
- All carbonated drinks may irritate the bladder.
- Fluid advice should also be part of the bladder training programme.
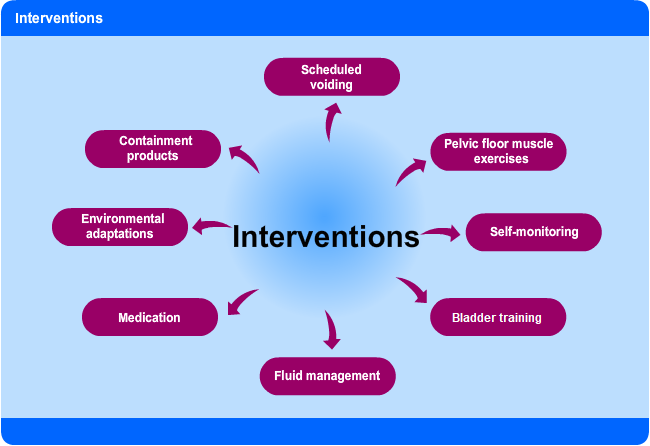
Interventions
Quality of life
The standardised validated questionnaire in the PDF can be used to identify bladder problems and/or urine leakage and the effects on the persons quality of life.
An example of a validated Quality of Life assessment tool
Investigations
| Investigations | |
|---|---|
| 1. Urinalysis | UTI (nitrates, leucocytes, protein, blood, pH), dehydration (specific gravity), diabetes (glucose, ketones). |
| 2. Post-void bladder scan/in-out catheter if scanner not available | Identifies persistent post-void residual urine volume. It is important to ensure the person empties their bladder before making a judgement about retention of urine.
Scanning should only be undertaken by a trained and competent practitioner. Common misdiagnosis:
|
| 3. Fluid balance chart and bladder diary | All should be recorded over 3 consecutive full 24 hour periods. Clear information is essential on: total voided volume, voiding frequency and timing, incontinence episodes and severity, functional bladder volume, episodes of nocturia/enuresis. Total fluid intake should be approximately 500mls more than output to allow for insensible loss. Types of fluid are important, especially the amount of caffeine containing drinks. Dehydration is common following stroke, especially if dysphagia present. |
| 4. Abdominal X-ray | Identifies constipation and faecal impaction |


