Category: Advancing Modules
Effects of stroke
Q. Match the skills, functions and abilities required to successfully use the toilet. Drag the functions from the list below to the correct description in the boxes. Each function may be used a number of times.
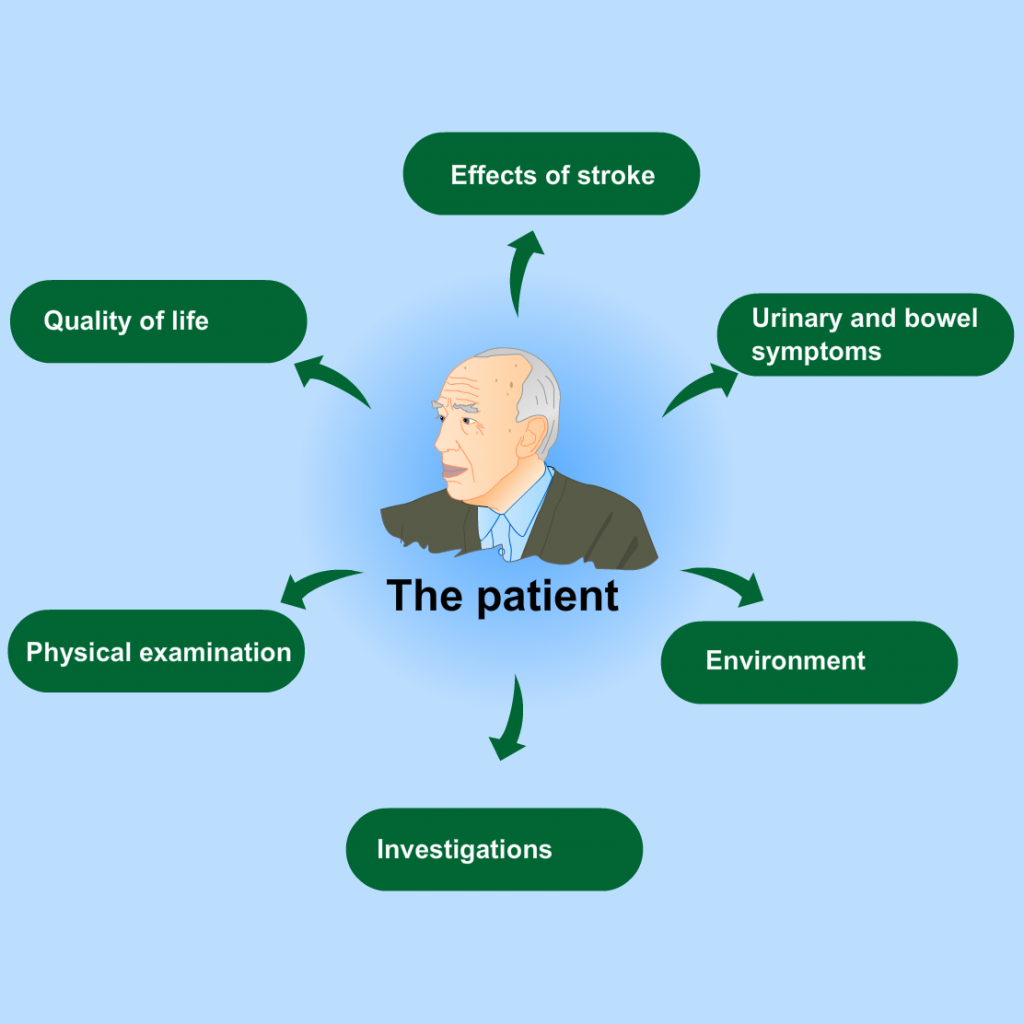
The patient
Select the crosses for more information.
Assessment
In the acute phase, or if a patient is acutely unwell, it may not be possible or appropriate to do a full bladder and bowel assessment. It should also be remembered that sometimes new onset bladder and bowel problems resolve spontaneously.
Assessment of bladder and bowel dysfunction, select the crosses for more information
Assessment and Intervention
Introduction
Assessment is key to both the quality and the outcomes of care. It is essential to understand the person’s needs in their personal living, health and family context. The specific type and nature of bladder and bowel dysfunctions experienced can only be accurately identified on the basis of a comprehensive assessment. Appropriate intervention is determined by the type of bladder and bowel dysfunction identified.
- Assessment
- Interventions
- Identifying type of urinary dysfunction after stroke
References
- Abrams P., Cardozo L., Fall M., Griffiths D., Rosier P., Ulmsten U., van Kerrebroeck P., Victor A. & Wein A. (2002). The standardisation of terminology of lower urinary tract function: report from the standardisation subcommittee on the International Continence Society. Neurourology and Urodynamics, 21, 167-178
- Brittain K, Peet S, Castleden C. (1998). Stroke and Incontinence. Stroke, 29, 524-528
- Patel M, Coshall C, Rudd A, Wolfe C. (2001). Natural History and Effects on 2-Year Outcomes of Urinary Incontinence After Stroke. Stroke, 32(1),122-127
- Clery A, Bhalla A, Rudd AG, Wolfe CDA, Wang Y. (2020). Trends in prevalence of acute stroke impairments: A population-based cohort study using the South London Stroke Register.
PLoS Med ,17(10), e1003366. https://doi.org/10.1371/journal.pmed.1003366 - O’Brien J, Austin M, Sethi P, o’Boyle P. (1991). Urinary incontinence: prevalence, need for treatment and effectiveness of intervention by nurse. BMJ, 303, 1308-1312
- Borrie M, Bawden M, Speechley M, Kloseck M. (2002). Interventions led by nurse continence advisors in the management of urinary incontinence: a randomized controlled trial Canadian Medical Association Journal, 166(10), 12671273
- Sultan AH, Monga A, Lee J, Emmanuel A, Norton C, Santoro G, Hull T, Berghmans B, Brody S, Haylen BT. (2017). An International Urogynecological Association (IUGA) / International Continence Society (ICS) Joint Report on the Terminology for Anorectal Dysfunction in Women. Int Urogynaecol J,2017,28 (1),5-31; Neurourol Urodyn, 2017, 36(1), 10-34
- Brittain K, Perry S, Shaw C, Mathews R, Jagger C, Potter J. (2006). Isolated urinary, fecal and double incontinence: prevalence and degree of soiling in stroke survivors. Journal of the American Geriatrics Society, 54, 1915-1919
- Getliffe K, Dolman M (eds) Promoting Continence, 2nd Edition, Balliere Tindall, London 2003
- Gray M. (2007). An update on the physiology of urinary incontinence Continence UK,1 (2), 28-36
- Anderson, Jamrozik, Broadhurst & Stewart-Wynne. (1994). Predicting survival for 1 year among different subtypes of stroke. Results from the Perth Community Stroke Study. Stroke, 25 (10), 1935-1944.
- Nakayama H, Jorgensen H, Pederson P, Raaschou H, Olsen T. (1997). Prevalence and risk factors of incontinence after stroke. The Copenhagen Stroke Study. Stroke, 28(1), 58-62
- Taub N , Wolfe C, Richardson E, Burney P. (1994). Predicting the disability of first-time stroke sufferers at 1 year. 12-month follow-up of a population-based cohort in southeast England. Stroke, 25 (2), pp. 352-7.
- Brittain k, Shaw C. (2007). The social consequences of living with and dealing with incontinence – a carers perspective Social Science & Medicine 1274-1283
- Cassells C, Watt E. (2003). The impact of incontinence on older spousal caregivers. Journal of Advanced Nursing, 42(6), 607-616
- Rotar et al. (2011). Stroke Patients Who Regain Urinary Continence in the First Week After Acute First-Ever Stroke Have Better Prognosis Than Patients with Persistent LUT Dysfunction. Neurourol. Urodynam, 30:1315–1318
- Tseng C-N et al. (2015). A Qualitative Study of Family Caregiver Experiences of Managing Incontinence in Stroke Survivors. PLoS ONE, 10(6): e0129540. doi:10.1371/
Impact of post-stroke incontinence
Q. Select Increased or Decreased for each of the questions below. Incontinence after stroke is associated with:
Types of post stroke continence difficulties
Non stroke causes of bladder and bowel dysfunction
Q. Match the non stroke causes of bladder and bowel dysfunction to the reason why.
Bowel control
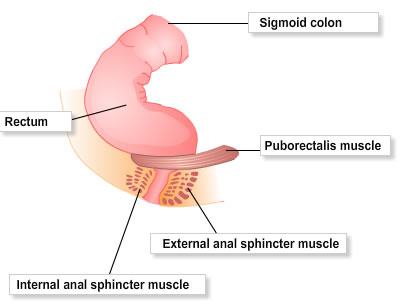
- Like the bladder the bowel is largely under autonomic control
- Emptying involves coordinated activity of the pelvic floor and anal sphincter muscles
- Faeces enters the rectum from the sigmoid colon, which stimulates the urge to defaecate via the recto-anal inhibitory reflex and the internal anal sphincter relaxes
- Valsalva’s manoeuvre increases intra-abdominal pressure
- The external anal sphincter and puborectalis muscle relax, which straightens the anorectal passage to aid bowel emptying
- Bowel emptying may be deferred by voluntary contraction of the external anal sphincter and pelvic floor puborectalis muscle, which decreases the ano-rectal angle and returns the mass to the rectum
- The internal anal sphincter relaxation reflex will fade after approximately 15 seconds and the urge to empty will resolve until triggered again


