Summary
Freda’s son has arrived from America and is reassured that his mother is being kept comfortable and that he can be with the family at her bedside for her last few hours.
Key Messages

- Decisions about alternative methods of providing nutrition and hydration should be reached using a shared decision making approach
- Shared decision making allows for possible treatment options, risks, benefits and evidence to be discussed with the patient and their family. The patient’s individual preferences, goals, values and beliefs can also be taken into consideration
- Learning methods of oral nutrition support. e.g the use of modified diet and fluids within stroke care, the use of a ‘food first’ approach and oral nutritional supplements to support poor dietary intake post stroke.
- The risk of Refeeding syndrome is high in patients who have nutrition recommenced following a period of over 5 days of nil or minimal intake.
- Assessment of a patient’s capacity is essential to their care planning and appropriate communication support should be provided when required
- Capacity is task specific and can change over time, thus the capacity status should be reviewed regularly
- Nasal retention devices and restraints eg. posey mitts may be indicated in some cases when there is repeated attempts to remove/dislodge NG tubes. Use of these should be considered on an individual basis and according to local protocols
- Ethical decisions around the provision of food and fluids in end-of-life care can be complex and the team need to respond to these on an individual basis

The goals of Freda’s care are to keep her comfortable. Offers of fluid and food may be appropriate if Freda is responsive to this and it does not cause her undue discomfort and distress.
The MDT work with the family to support her end of life care.
For information and learning on end of life care visit STARS AM 16

Freda is now not rousable and has had another CT scan which has shown she has had a further stroke.
The team review their original plan to NG feed Freda for 2 weeks and decide to provide palliative care. For this reason further attempts at NG placement will not be pursued.
Nasal Retention Device

A nasal retention device is a piece of equipment to secure a tube, such as NG in place. The use of a tube can promote safer practice and ensure that feeding is delivered and avoiding complications of repeated removal or dislodgement of tubes.
Posey mitts

Posey Mitts are used as a method of restraint to prevent patients from injuring themselves by pulling or removing NG tubes that are being used as part of their treatment.

Ponder point: consider the ethics around their use. Do you think they are appropriate for cases like Freda?
Here is an example of a guideline for the use of posey mitts and nasal bridles that we use at Gourmet General Hospital.
Attempting to involve Freda in the decision about her feeding should be the first step.
Capacity is task specific and she may have sufficient understanding to decide on her feeding and be able to communicate this with appropriate assistance.
To determine capacity you need to know if Freda can:
- Understand the purpose of the feeding tube
- Understand that there are benefits and risks for her
- Retain the information or show consistency in her response
- Be able to communicate her decision in a reliable way

Taking time to present this information in different ways such as written, pictorial and with spoken explanation and then allowing her to make choices will help Freda determine her own care.
It has been determined that Freda does not have the capacity to make decisions. The MDT including the family have agreed to continue with NG feeding and are looking at ways to maintain the NG tube placement.
Despite being quite drowsy, Freda is managing to remove her NG tube several times a day.
It is day 3 post-admission and you are commencing Freda’s nasogastric feeding regimen. However, she may be at risk of refeeding syndrome.
Freda is assessed to be at LOW risk of refeeding syndrome as she was eating normally pre-admission, she has been nil by mouth for 3 days since admission, she has not lost significant weight, her BMI is >18.5kg/m2 and her electrolytes are within range.
The consultant has completed an incapacity certificate for Freda regarding her NG feeding. Click here to view the completed incapacity certificate.
Freda’s incapacity certificate [32KB]
NB: There may be local or national variations to incapacity certificates.
The consultant is meeti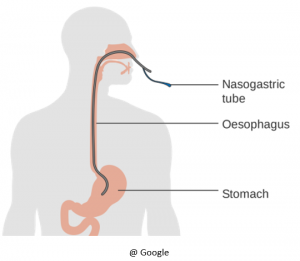 ng with Freda and her daughter to discuss how best to provide Freda’s nutrition & hydration.
ng with Freda and her daughter to discuss how best to provide Freda’s nutrition & hydration.
He explains that the following has been considered:
- MDT assessments
- Comments from family
- Freda’s current condition – she is now stable, brighter and managing to say a few words
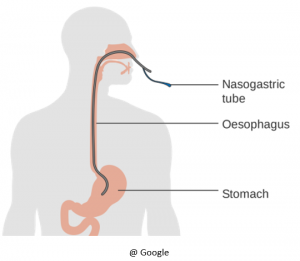
He goes on to explain that the team feel they would like to feed Freda using a nasogastric (NG) tube. This could be trialled for 2 weeks to optimise Freda’s recovery. He explains the risks and benefits of providing both nutrition and hydration in this way and invites comments from the family.
They family agree to NG feeding and are happy that the intervention will be reviewed in 2 weeks.
![]()






 ng with Freda and her daughter to discuss how best to provide Freda’s nutrition & hydration.
ng with Freda and her daughter to discuss how best to provide Freda’s nutrition & hydration.