Bill is feeling a bit anxious about having an NG tube inserted and would like some further information. To reassure Bill and help him to understand what this involves, the nurse explains the procedure to Bill:
- A nasogastric tube is a thin tube that will be inserted into your nose and it will reach down to your stomach.
- What I am going to do first is measure the NG tube against your body so that I know how much of the tube needs to be inserted.
- I will hold the tube and measure the distance from your nose to your stomach and put a small mark on the tube.
- I will lubricate the tube to help it go down. I will then insert it into your nostril and pass it down to the back of your throat. This may be a little uncomfortable.
- I will ask you to open your mouth so that I can check the tube is going down and not coiled up in your mouth.
- Once the tube is into the stomach I will secure it in place using a secure tape for your nose.
- I will then take a syringe and attach it to the end of the tube and will draw back some of the liquid from your stomach. This is a test to see it is in the right place and we will do this test every time we start a new feed or before we put medication into your tube.
- You may be sent for a check chest x-ray to make sure the tube has been placed correctly. This is for safety reasons as sometimes tubes can be incorrectly placed or can be dislodged and we do not want to feed you if it is in the wrong place.
- This type of tube can stay in for between four to twelve weeks depending on NG tube type.
- If a tube is needed for longer than this we will discuss this with you in due course.
 Bill feels reassured by this explanation and consents to the NG tube insertion. He is given an information leaflet on NG feeding that can be shared with his family.
Bill feels reassured by this explanation and consents to the NG tube insertion. He is given an information leaflet on NG feeding that can be shared with his family.
NB/ This is an explanation for Bill and does not constitute training for staff on NG insertion. For full procedural information on how to pass an NG tube, see your local guidelines.
There are some factors which should be carefully considered when determining if someone is suitable for NG feeding.
None of these apply to Bill and he will have his NG tube passed this afternoon.
NB: Practitioners must be competent in placing a NG tube (and nasal bridles if applicable).
Bill attends the x-ray department for his videofluoroscopy and is given a small amount of food and fluid of different consistencies, mixed with a contrast material such as barium. The moving image allows the SLT to track the pathway of the food/fluid through the oral cavity and pharynx and detect any signs of a swallowing impairment at these levels.
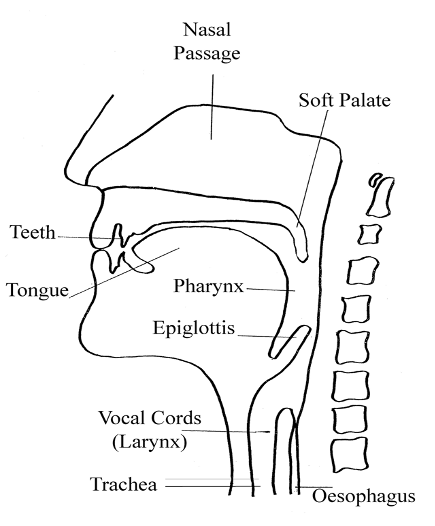
The diagram below shows the anatomical structures required for swallowing.
Video by kind permission of Nutricia.
(This video contains sound, please ensure that the computer you are using has sound enabled and speakers or headphones. You can enlarge the video by clicking on the enlarge icon in the control bar under the video clip. Please note: videos may not load if you are accessing these through an NHS firewall.)
Bill has difficulty clearing his pharynx. The pharynx is the back of your throat. It sits behind the mouth, below the nose and above the trachea (airway) and oesophagus (gullet).
Can you spot the moment when Bill aspirates? A person should cough to expel the material from their airway but a cough reflex may be delayed or absent after a stroke. If the cough reflex is not triggered, this is known as silent aspiration.
The outcome of his videofluoroscopy shows that Bill is unsafe to swallow all oral diet and fluid consistencies at this time. The MDT, in discussion with Bill and his family, decide as a first step to pass an NG tube. The Speech and Language Therapist will continue to review Bill’s swallowing status and devise a swallowing therapy programme for him.
As per the Scottish Stroke Standards, Bill has had his swallow screen within 4 hours of admission to hospital, and is deemed safe to eat and drink. Later in the day, however, there are signs that Bill’s swallow has deteriorated. You are concerned that his swallow may now not be safe.
The swallow screening test is not sensitive enough to pick up every swallowing impairment. Aspiration is when the food or fluids enters the airway below the level of the vocal cords. It is important to closely monitor the patient when they resume eating and drinking and monitor for signs of aspiration/deterioration in chest status.


Bill has presented at A & E after his wife found him unsteady on his feet, complaining of double vision, and slurring his words when he got up from the breakfast table. She recognised the FAST symptoms and phoned for an ambulance immediately. He has a history of hypertension and stopped smoking 12 months ago.
Summary
Over time, Connie’s swallowing ability has improved and she is now managing a Level 7 food (easy to chew) and Level 0 drinks (thin) from an open cup. She is now able to meet her needs from oral food and drinks alone. Her weight has been maintained whilst in hospital and she is due to be discharged home next week.
Key messages:
- A patient’s swallowing ability should be reviewed on a regular basis to monitor for changes in status
- All patients should have a nutritional risk assessment (i.e. MUST) carried out on admission to hospital and repeated at regular intervals
- It is important to determine exactly what consistencies of food/drinks have been recommended to a patient and what food choices these constitute
- Any additional information given by the SLT on strategies, equipment and positioning for swallowing should be adhered to
- The eating and drinking environment should be adapted to create a safe and optimal nutritional opportunity, encouraging both physical independence and nutritional autonomy with meal choices
- Stroke patients on modified diets are at increased nutritional risk and may require fortification or supplementation of their diet
- Accurate monitoring of patients food and drinks intake is important to allow adjustment for changes in the prescribed therapy
- It is good practice to involve / inform the patient and carers in the management process and keep them regularly updated and involved.
It is important to be able to measure the impact of any clinical intervention, in this case Connie’s nutritional care plan.
The Dietitian has asked for food and fluid charts to be completed. This will allow a calculation of her diet and fluid intake and help to ascertain if Connie is meeting her nutritional requirements. It is important that these charts are completed as accurately as possible to allow an informed evaluation to be carried out.
Accurate food and fluid charts should include:
- specific quantities of foods taken, e.g. ½ bowl porridge, 1 yoghurt
- specific quantities of fluids taken, e.g. 200ml tea, 150ml mil
- any diet or fluid refusal including any known reason for this
- intake of ONS including type and quantity
ONS are frequently recommended by Dietitians as a way to increase individuals intake who cannot meet their needs from food alone. They are prescribed based on the patients needs including, swallow recommendations, taste preferences, patient abilities and nutritional need.
A wide range of products are available. They come in a variety of types including milk based, juice based, yoghurt based and also come in different sizes.
The dietitian has recommended that Connie should have 1 x compact milk based supplement per day.
Take some time to consider:
- Taste preferences and how this could impact on ONS chosen
- Temperature of ONS provided i.e. was it given at room temperature or from the fridge
- Timing of ONS – was it given first thing in the morning after waking or mid day?
How could these factors affect Connie taking her prescribed ONS?
Snacks are an important way of increasing nutrition throughout the day. Eating occasions do not need to be limited to meal times only. Very often patients will tire quickly when eating and this restricts the amount that they are capable of achieving at one sitting. Increasing the opportunities to eat or drink through the day can improve intake.
- Encourage to eat little but often
- If someone takes very small portions- offer them a small snack and nourishing drink between meals
- Snacks and fluids between meals need to follow SLT recommendations
Click the link for further information and ideas on a food first approach.
 Bill feels reassured by this explanation and consents to the NG tube insertion. He is given an information leaflet on NG feeding that can be shared with his family.
Bill feels reassured by this explanation and consents to the NG tube insertion. He is given an information leaflet on NG feeding that can be shared with his family.