Temperature, Respiratory Rate and Oxygen Level
Archie is a 69-year-old retired accountant who was admitted to hospital after waking from sleep with loss of speech and weakness down his right side. The exact time of onset was unclear and he was admitted to the stroke unit five hours after wakening. A number of observations were carried out on admission to the stroke unit, which are shown in the chart.
Q. Are Archie’s results normal? Select either normal or abnormal for each result below.
In this case it is expected you will now have an understanding of:
- The potential and pathophysiological harm of hyperglycaemia in acute stroke patients
- Recognising the high incidence of increased glucose in acute stroke patients.
- The method and frequency of blood glucose monitoring
- The urgency of rapid intervention to correct hypoglycaemia

Six months after his stroke Bob is feeling much better and during a routine check up at his local surgery he mentions that he’s keen to return to driving. Bob’s GP refers him for a formal driving assessment, which he passes. Bob is now busy making plans to go and visit his sister who lives in Thurso. Bob has also found it very helpful to work through the CHSS self management resource: Selfhelp4stroke.
Over the next few days Bob improved and his glucose was controlled with oral hypoglycaemics. He is due to leave the acute stroke unit and announces “nobody has told me anything about diabetes“.
What information and explanation would you give Bob? Think and list some of things you would do before turning to the next page for some answers.
You come on shift the next morning and notice that Bob is pale and sweaty, dizzy, shaky and appears confused with a GCS of 14/15.
On day three after his admission Bob has a large hospital meal, plus a large box of chocolates, despite the nurses previously giving him some dietary advice. The next routine BM stix shows his glucose to be even higher at 16mmol/l. The doctors decide that this needs to be better controlled and decide to start Bob on an insulin sliding scale.
Example of a Diabetic Control Table. NB: These will vary so please refer to your local charts.
Patient name:
|
Bob Ferguson
|
DOB: 23/03/62
|
Consultant:
|
Dr Ross
|
|
| Date |
21/11/2020 |
21/11/2020 |
21/11/2020 |
21/11/2020 |
21/11/2020 |
| Time |
07:30 |
09:30 |
11:30 |
13:30 |
15.30 |
| Insulin Name and Units |
|
| Actrapid |
|
|
|
|
|
| as per BM |
4 |
3 |
3 |
2 |
2 |
|
|
|
|
|
|
| Signature: D. Ross |
D Ross |
D Ross |
D Ross |
D Ross |
D Ross |
| BM results (mmol/L |
16.0 |
13.8 |
12.2 |
10.7 |
10.2 |
| Ketones |
|
|
|
|
|
Insulin sliding scale prescription
| Drug/Dose
Actrapid 100units in 100ml
0.9% Saline |
BM result
(mmol/L) |
Insulin rate
(ml/hr) |
| 0 – 4 |
0 |
| ROUTE Intravenous |
5 – 7 |
1 |
| 8 – 10 |
2 |
| Start Date
21/11/2020 |
Doctors Signature
Doug Ross |
11 – 15 |
3 |
| 16 – 20 |
4 |
| Disc. Date |
Doctors Signature |
21 – 28 |
6 |
| >28 |
Inform Dr |
An insulin sliding scale is a temporary measure to control glucose levels in acute stroke patient with very high blood glucose (>15 mmol/L). It involves intravenous administration of a standard insulin to tightly regulate blood glucose levels. Blood glucose levels are monitored using bedside, finger-prick capillary glucose monitoring machines. The rate of infusion of insulin is titrated according to the glucose which is ideally monitored every 1-2 hours. Insulin given intravenously has a short half-life of a few minutes.
Q. How common is abnormal glucose and diabetes in acute stroke patients? Answer Yes or No to each of the questions below:
For more details on quiz answers see additional information
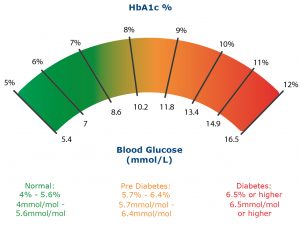
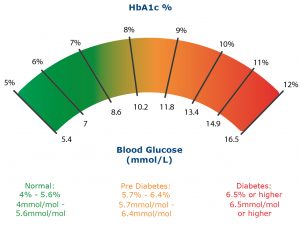
You look at the computer and notice that Bob’s HbA1C level is over 48mmol/mol (over 6.5%).
Q. What does this indicate? Answer Yes or No to each of the questions below:
As Bob’s capillary blood glucose (CBG/BM) was 10.8 mmol/l. what would you do next? Select Yes or No for each question. Correct answer in Bold
![]()