Category: Advancing Modules
The challenges
The most reliable evidence on which to base decisions comes from the randomised trials assessing thrombolysis and thrombectomy. These have clearly shown that both treatments can improve selected patient’s functional outcomes and that the interval from stroke onset to treatment is the major determinant of the size of the potential benefit:
Thrombolysis within 3 hours produced 10 additional good outcomes /100 treated, if the delay was 3-4.5 hours only about 5 good outcomes /100 were achieved – so 5 fewer patients have a good outcome per 100 treated:
Thrombectomy within 6 hours produced 40 patients with less disability /100 treated but for every additional hour of delay to thrombectomy – 7 fewer patients have a good outcome per 100 treated.
Many factors have been associated with worse outcomes after treatment –e.g. increasing age, increasing stroke severity, high blood sugar, very low or high BP, but they are often associated with poor outcomes even in the absence of treatment and may not influence the size of the treatment effect.
The presence of some factors such as oral anticoagulation, very high blood pressure, recent trauma or operation excluded patients from RCTs so that we have little robust evidence on which to judge the extent to which they might reduce the effectiveness of the treatments. We often have to rely on uncontrolled observational studies which have a high risk of producing biased results.
Approach to decision making
The decision to treat with thrombolysis and/or thrombectomy should be based on an individual assessment of the patient’s likely benefits and risks.
- The benefits are a reduced likelihood of having persisting deficits which will disable the patient
- The risks of thrombolysis have been described in the hyperacute stroke treatments module: 01 Hyperacute stroke treatments including thrombolysis and thrombectomy: Case: 3 Angela
- The risks of thrombectomy have been described in the hyperacute stroke treatments module: 01 Hyperacute stroke treatments including thrombolysis and thrombectomy: Case: 4 Iain
- Most conservatively you might apply strictly the eligibility criteria in the alteplase datasheet. However, relatively few patients will fulfil these.
- The American Heart Association guidelines include a fairly exhaustive list of recommendations regarding the eligibility for treatment with iv thrombolysis, but leaves many judgements to be made by the physician treating the individual patients. See table.
- Many physicians treat patients who do not strictly meet all the criteria. They might treat a patient who has several very favourable factors e.g. very short delay since onset, no uncertainty about diagnosis, young age but has some relative contraindication e.g. operation one month before.
- Clinicians need to weigh up the relative importance of each factor and then taking account of the patient’s, or their family’s, views to reach a final decision about whether to offer thrombolysis and/or thrombectomy or not.
Making the decision to treat

Aims of module
- To understand the factors which clinicians use to determine the balance of benefits and risks associated with thrombolysis and thrombectomy in acute ischaemic stroke.
- Provide clinical cases to enable clinicians to practice their assessment of clinical and radiological information which they need to take account of.
- Provide clinical cases to enable clinicians to practice their decision making with respect to thrombolysis and thrombectomy, and compare their decisions with those of experienced stroke physicians.
02: Experienced colleagues decisions
Select the crosses for each colleagues decision and rationale
02: Update and decisions
Now 3 hrs 40 mins (220 mins) since onset, BP currently 150/76, NIHSS unchanged at 10.
02: CT Angiogram
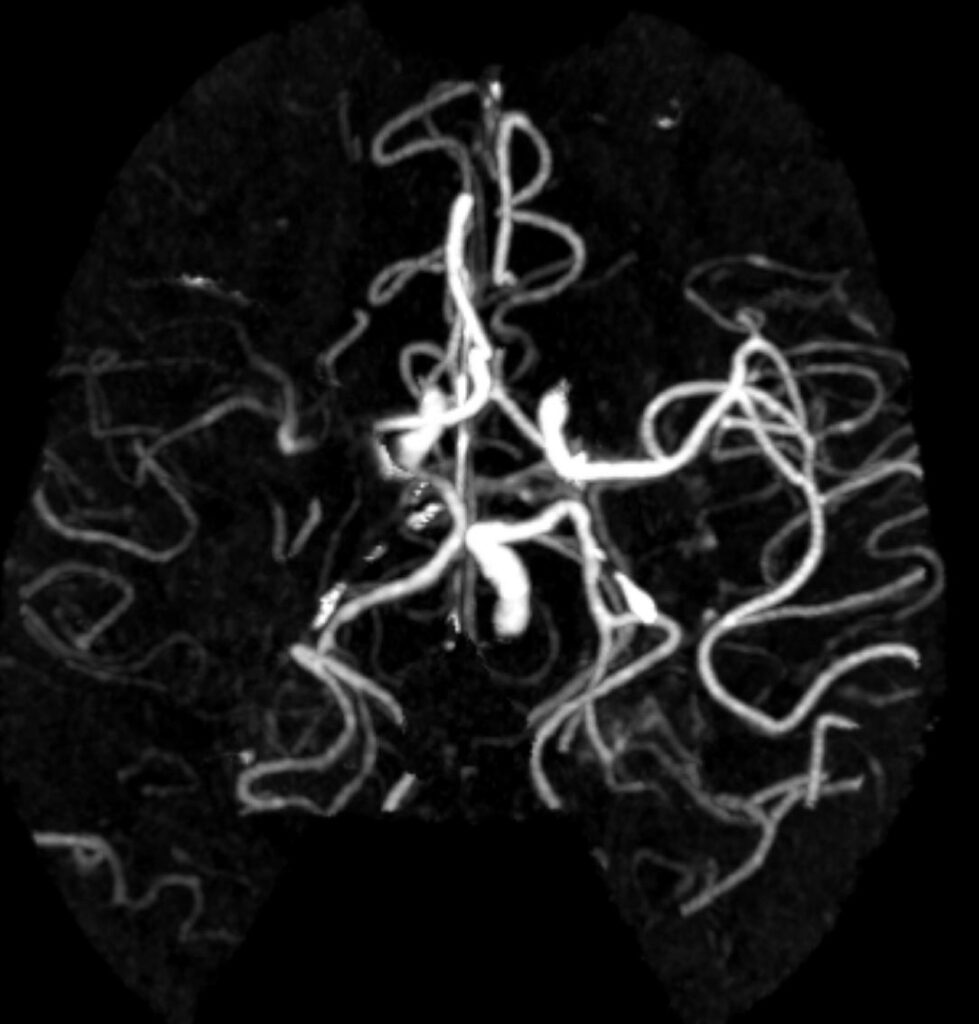
What abnormalities if any can you see?
02: Non contrast CT head
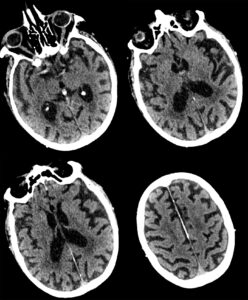
What abnormalities if any can you see?
Case 02
Clinical history and examination
Age: 75 years, Male.
Time of presentation: 08.30
History of event
- Symptoms: at breakfast wife noticed left face droop, slurred speech and weak left arm
- Current time interval since last known well: 3 hrs 20 mins (200 mins)
Past medical history
- AF
- Previous minor strokes
- Moderate cognitive deficits
Relevant medications
- Bisoprolol
- Apixaban: last taken that morning
Relevant social history
- Living circumstance: living at home, with wife
- Prior function and care needs: mobile but needs supervision of most daily activities – mRS 3
- Work/hobbies: retired joiner, watches TV, walks the dog
Examination
- Pulse: 80 irreg, BP: 140/80
- Neuro:
- Handedness: left handed
- NIHSS: 10
- Deficits: left face UMN weakness, moderate dysarthria, flaccid left arm with inattention
Investigations requested with non imaging results
- ECG confirmed AF


