Flushing
Flushing of the tube is essential for 2 very important reasons:
Tube patency – Regular flushing of fine bore NG tube is important to maintain tube patency. This may be a patients sole access point for fluid/ medications. Fine bore tubes can block easily and require regular flushes.
Fluid volume – The regimen for feeding may be arranged to allow sufficient fluid to be administered. This takes into account flushes between bottles and with frequency of medications.
Troubleshooting and Tolerance Issues
Monitor for signs of poor tolerance of the feed and discuss these with the dietitian, prior to alteration of feed regimen. Symptoms may be related to other reasons, e.g. infection, underlying health conditions, medications, rather than feeding regimen.
| Symptom |
Influencing factors |
Possible Intervention |
| Nausea
Vomiting
Reflux
Abdominal pain
Abdominal distension
Diarrhoea
Constipation
|
Polypharmacy (sorbitol)
poor hygiene practices
suboptimal method of feeding e.g. pump or bolus
timing of feed, e.g. day or night
hourly feeding rate
medications
vertigo
movement
feed temperature
change in position of NG tube/tube migration
fibre content of feed
concentration of feed
volume of feed
volume of water flushes
incorrect fluid balance
|
Review Medications
Ensure good hygiene practice is followed when connecting/disconnecting feeds
Do not use feed bottle for >24 hours once opened
Confirm NG position
Ensure feed at room temperature
Change method of feeding
Change timing of feeding
Change rate of feeding
Change fibre content of feed
Change concentration of feed
Change feed volume
Change water flushes
Stop feed prior to movement/therapy input |
Any changes to feeding regimes, should only be done following MDT discussion with dietitian.
https://www.bapen.org.uk/nutrition-support/enteral-nutrition/complication-management
 The dietitian will undertake an assessment of nutritional status and current clinical condition. The regimen is tailored to meet individual needs based on a persons’ specific nutritional requirements and goals of the intervention. It is individual to the patient in terms of need for energy, protein and fluid, as well as micronutrients.
The dietitian will undertake an assessment of nutritional status and current clinical condition. The regimen is tailored to meet individual needs based on a persons’ specific nutritional requirements and goals of the intervention. It is individual to the patient in terms of need for energy, protein and fluid, as well as micronutrients.
The product has been specifically chosen and should not be replaced with an alternative without prior confirmation.
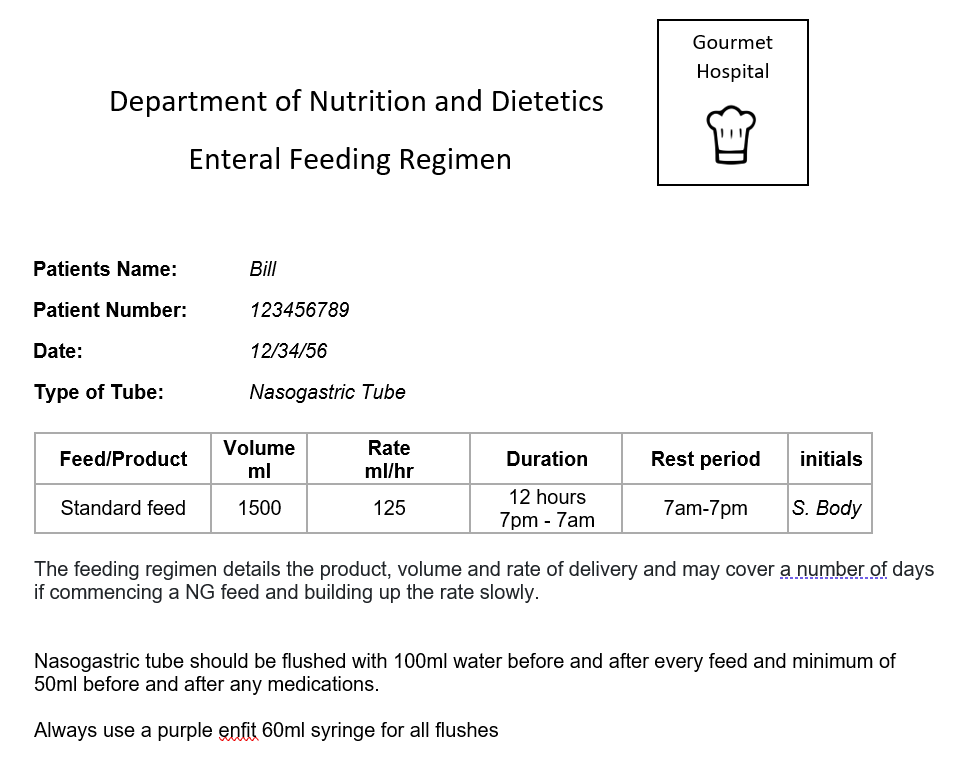
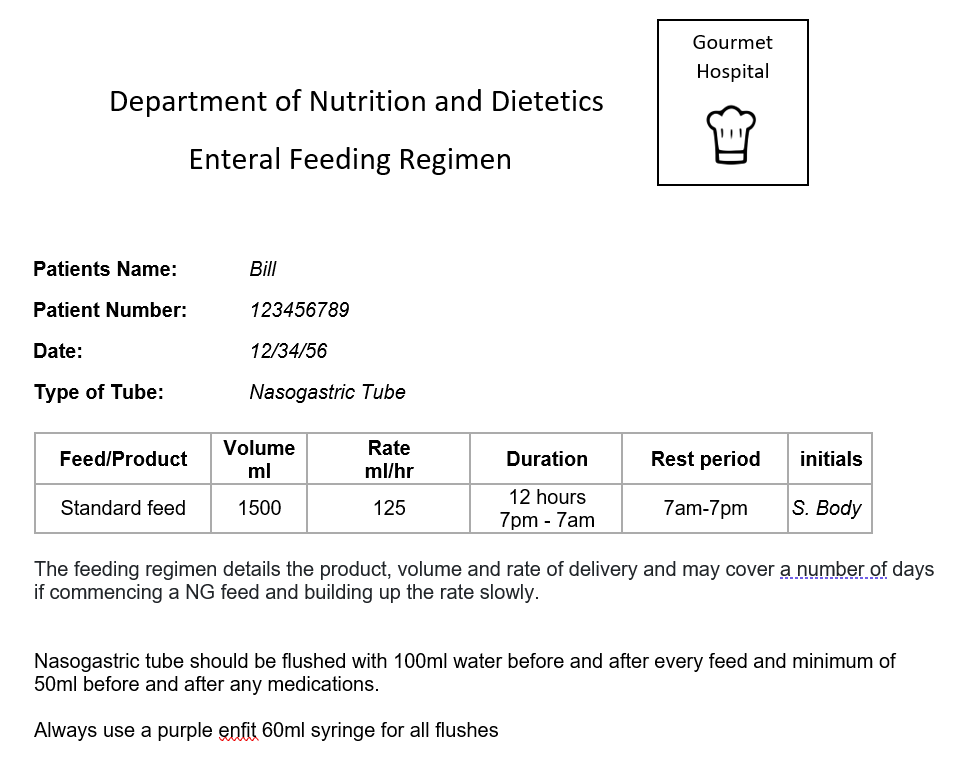
The feeding regimen details the product, volume and rate of delivery and may cover a number of days if commencing a NG feed and building up the rate slowly.
Bill has had his swallow screen completed by the nursing staff and has been reviewed by a Speech and Language Therapist who has completed his swallow assessment. Bill is not recommended to have any oral food or fluids currently and is nil by mouth (NBM)
When a person’s swallowing is unsafe or under review by a Speech and Language Therapist, there are a number of alternative hydration and nutritional options available for consideration. Each case should be considered on an individual basis taking into account the individual’s acute medical state, consent and cognition.
Bill and his family would like to know what options are available to him regarding his nutrition and hydration if his swallow remains unsafe.
| Nutrition and hydration options |
| Oral intake |
If the swallow screen and swallow assessment are safe oral intake should be started. The person should be observed and the SLT will recommend a textured diet if required |
| Intravenous infusion (IV) |
This only provides fluids and will not provide you with any of the nutrition you need. This is a short term option |
| Subcutaneous infusion (SC) |
This only provides fluids and will not provide you with any the nutrition you need. This is a short term option and may be used when venous access is difficult or when small volumes of fluid are needed for comfort e.g end of life |
| Nasogastric feeding (NG) |
If oral intake is insufficient and likely to be so for > 1-7 days. This is the placement of a tube through the nose, down the throat, and into the stomach. It is usually the first option for feeding somebody who has had a stroke, if they are unable to swallow. |
| Gastrostomy
(e.g. PEG) |
This is considered if a NG has been in place for 3-4 weeks and there is little or no improvement in their swallowing ability. This is done by endoscopy and requires sedation. A tube is placed directly through the stomach wall and into the stomach to provide food and fluids. |
| Parenteral Nutrition (PN) |
This is a type of feeding directly into the person’s vein, bypassing the usual process of eating and digestion. It is only used if GI tract is not accessible or functioning. |
| Eating and drinking with accepted risk |
In some circumstances, artificial nutrition and hydration is not wanted or appropriate, therefore there is an option to eat and drink with accepted risk. This may be chosen when the patients quality of life would be affected by not eating and artificial nutrition may not enhance their quality of life. The risks include choking on diet and fluids which can be serious and life threatening. This is discussed with patients, families and their healthcare team when appropriate. |
The Speech and Language Therapist has a discussion with Bill and his family about carrying out a videofluoroscopy, an instrumental assessment using x-ray equipment, to provide a more detailed assessment of the swallow and Bill consents to this.
Rosemary has identified her financial situation as a concern as she prepares for discharge home. Let’s look at how she can be supported at this stage:
- Signpost/ support for financial assistance
- Help Rosemary to understand the benefits of work to her health
- Support to engage with her employer
Financial stress has been identified by Rosemary as her immediate concern. You could encourage her to discuss this with her husband / support network. Rosemary may be entitled to benefits, so you could signpost her to mygov.scot/benefits-support or local citizens advice.
Although Mr McTavish has increased tone distally in the left arm, he also has a low-toned subluxation at the shoulder. His positioning and handling strategy needs to take this into account and as near normal anatomical alignment of the glenohumeral joint should be maintained during all movements. Mr McTavish should always have the left arm well supported by pillows and/or table.
Management plan- To reduce and further prevent hemiplegic shoulder pain by:
- Providing adequate support for upper limbs
- Providing appropriate positioning of upper limbs using pillows, lap trays, positioning charts
- Careful handling of the upper limb through pain free range
- Educating the patient to self care for the affected upper limb
- Prescribing appropriate analgesia
- Discussing management strategies with MDT to ensure a coordinated and consistent approach
Mr McTavish has left homonymous hemianopia and left visual inattention. Most stroke patients push towards the hemiplegic side because they fear falling to the unaffected side (i.e. where they perceive the danger of falling to be). Providing adequate base of support on the unaffected side will reduce the tendency to push. Mr McTavish tends to use his right arm and hand, and his right trunk muscles to fix himself on this side in sitting which orientates him toward his non-affected side and causes him to be asymmetrical. He needs to be positioned so that he receives stimulation from the left and with his weight distributed evenly.
Management plan- To re-orientate the patient to the mid-line by:
- Using appropriate positioning
- Providing adequate base of support
- Approaching the patient from their affected side
- Providing stimulation on their affected side
- Explaining to the patient the rationale for these management strategies to maximise compliance
- Discussing management strategies with MDT to ensure a coordinated and consistent approach
Mr McTavish has intact gross touch on the left side of the trunk, and the proximal lower limb. He has absent tactile sensation in the left arm and hand. He cannot feel the left side when the right side is touched simultaneously. This has implications for the overuse of the unaffected side, and he may quickly lose function in his affected side.
Mr McTavish can feel movement in the left leg and can accurately describe the positions of his left hip and knee. He cannot detect movement or the position of his left arm.
Management plan:
- Care must be taken when handling and positioning limbs with altered sensation and proprioception as patients will often be unaware of the risk of trauma to the limb
- Explain to the patient the importance of protecting their limbs
- Provide appropriate tactile sensory feedback through handling and base of support e.g. pillows, towels, cushions etc
- Encourage the patient to be functionally independent as appropriate
- Prior to carrying out a weight-bearing transfer, ensure that the affected foot is well-aligned on the footplate, or floor, and that the ankle is stable
- Discuss management strategies with MDT to ensure a coordinated and consistent approach
Mr McTavish presents with:
- Shoulder: ½ normal range of flexion, ½ abduction and ⅓ lateral rotation, limited by pain.
- Elbow: Full range of movement (FROM)
- Wrist: Limited combined wrist & finger extension due to shortening in the long finger flexors as a result of increased tone
Mr McTavish has no active movement in the upper limb (Grade 0), he has proximal Grade 3 movement in the lower limb (hip flexors and extensors, knee extensors) and grade 2 movement distal to the knee.
Management plan- To maintain and improve joint movement by:
- Performing regular passive movements within normal anatomical, pain free range
- Using base of support and alignment to allow the patient to maximise their movement capabilities
- Encouraging the patient to be functionally independent as appropriate. Sometimes patients should be discouraged from attempting things which require a lot of effort since this can increase tone.
- Explaining the importance of maintaining flexibility of muscles and joints to the patient to maximise compliance
- Discussing management strategies with MDT to ensure a coordinated and consistent approach
 The dietitian will undertake an assessment of nutritional status and current clinical condition. The regimen is tailored to meet individual needs based on a persons’ specific nutritional requirements and goals of the intervention. It is individual to the patient in terms of need for energy, protein and fluid, as well as micronutrients.
The dietitian will undertake an assessment of nutritional status and current clinical condition. The regimen is tailored to meet individual needs based on a persons’ specific nutritional requirements and goals of the intervention. It is individual to the patient in terms of need for energy, protein and fluid, as well as micronutrients.