Module test



Having completed this module you should now have a critical understanding of:
Vera was repatriated on the day after her thrombectomy. She recovered well, and went home a week after her stroke, able to live independently and care for her husband.
Vera had a thrombectomy, unblocking her right middle cerebral artery (MCA). She is transferred to the hyperacute stroke unit after waking up from the general anaesthetic in recovery. The nurses monitor her condition carefully (see Iain’s story).
Vera is much better (mild facial weakness and mild drift of arm and leg, normal visual fields and slight inattention of left) the following day. Her NIHSS has improved from 15 before transfer to 4.
The stroke physicians assess her progress twice daily to determine when she might be fit for repatriation.
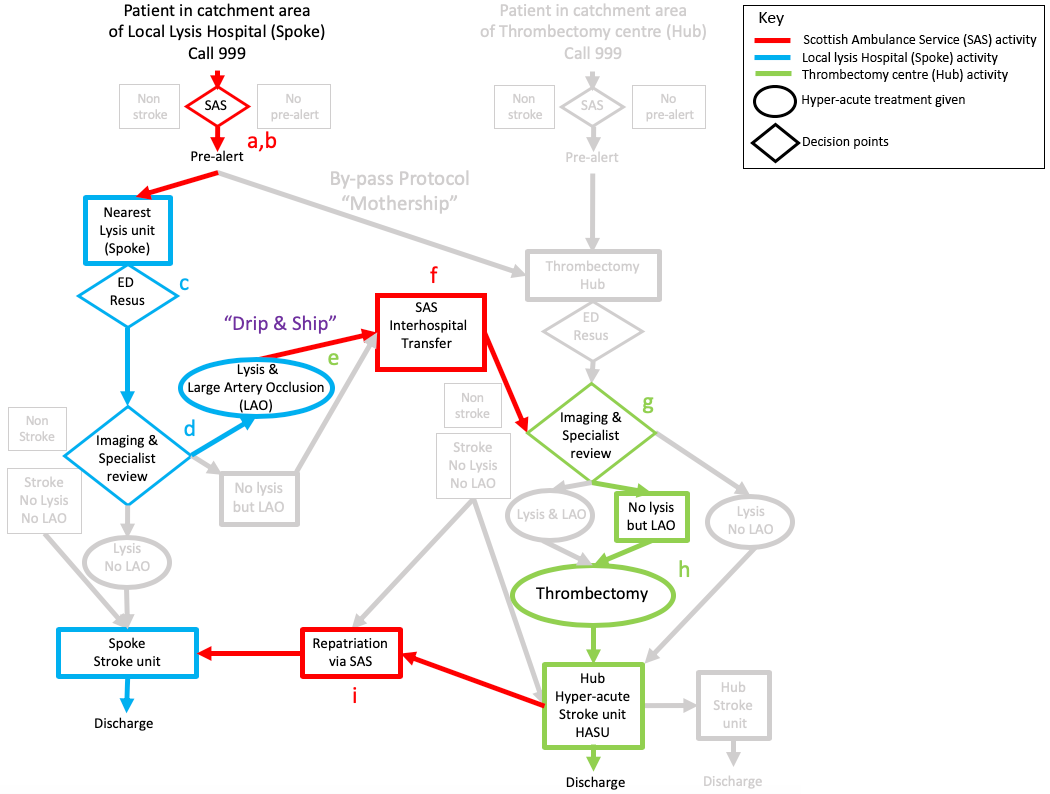
Vera arrives at the thrombectomy centre and is taken straight to the Radiology dept (not ED since she has already been through the first part of the pathway at the spoke hospital). She is met by the team comprising the INR, anaesthetist and hub stroke nurse. The paramedics give a verbal handover.
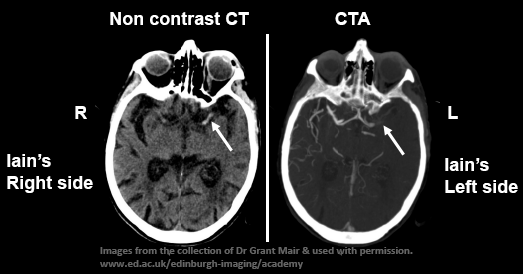
Brain scans by Grant Mair is licensed under CC BY-NC-SA 4.0
Iain’s non-contrast CT scan excludes a bleed but shows a dense (white) middle cerebral artery (MCA) on the left due to clot within the artery. There are also some early ischaemic changes (loss of grey/white matter discrimination) visible. A blocked proximal MCA is confirmed on the CTA (arrow).
The NIHSS is an internationally accepted tool for the systematic assessment of stroke severity. It comprises a 15-item neurological examination stroke scale used to evaluate the effect of an acute cerebral event on the levels of consciousness, language, neglect, visual-field loss, extra-ocular movement, motor strength, ataxia, dysarthria and sensory loss. It can be used by appropriately trained healthcare professionals and takes approximately 10 minutes to administer. However, the whole NIHSS does not need to be completed to make the initial diagnosis or to decide that hyperacute treatment would be indicated. It can be completed whilst waiting for the scans. The use of such an assessment tool ensures that a standard range of neurological signs and symptoms can be measured consistently over time providing a basis for clinical decision-making. Patients may not be suitable for thrombolysis (NIHSS<4) or thrombectomy (NIHSS<6) if the stroke is mild and not causing the patients difficulties.
Click the link below to complete the free NIHSS online training:
BlueCloud: Individual Memberships for Healthcare Professionals
All staff (stroke nurses and medical staff) involved in the management of hyperacute stroke patients should have completed training in the use of the NIHSS and be proficient in its use. Watch the video below and score the patient on the NIHSS. You might find it useful to open up the NIHSS assessment form below.
Try filling in a version of the form for yourself: Interactive NIHSS score sheet [.pdf, 955KB]
Video provided by kind permission: Mark Garside – Northumbria Healthcare; Chris Price – Newcastle University.
Duration: 4 minutes 58 seconds
The ambulance arrives at the spoke hospital at 10.40.
The 60min alteplase infusion only started at 10.20. The spoke stroke physician has to make the difficult decision based on an assessment of risks and benefits whether to:
In this case the stroke physician decides to stop the infusion because no nurse is available to accompany the patient and the delay to thrombectomy may be reduced by at least 30 minutes. Had the patient been treated with Tenecteplase which is given as a single bolus no infusion would have been required (link back to “What is thrombolysis?”._
Vera is transferred into the ambulance by the paramedics. No nurse or anaesthetist is required for this transfer.
The family or next of kin do not travel in the transfer ambulance. Vera’s daughter drives John, Vera’s husband, to the thrombectomy centre.
Estimated transfer time: 1 hour.