The patient will be in the ambulance without any relatives.
Paramedics
- Responsible for overall patient care during transfer.
Stroke nurse
- A nurse is only required if a decision has been taken to continue an infusion of alteplase, or blood pressure lowering medication. which requires an infusion pump – paramedics are not currently trained in the care of infusion pumps.
Anaesthetist
- An anaesthetist is only likely to be required in a patient in whom there is a significant risk of reducing level of consciousness (e.g. severe posterior circulation stroke). This will be decided at the spoke.

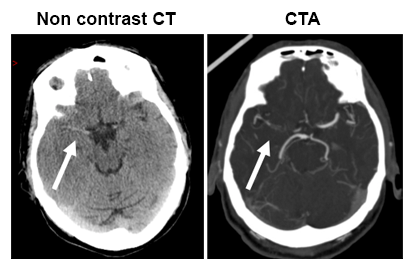
The senior clinician responsible for Vera reviews her eligibility for thrombectomy. They confirm that Vera was previously independent, has a definite new ischaemic stroke with deficits severe enough to warrant thrombectomy and a large artery occlusion on the CTA. (See Eligibility for thrombectomy Word .doc)
The stroke physician phones the regional thrombectomy hub to discuss Vera with the hub stroke physician who reviews the CT/CTA on the national picture archiving and communication system (PACS) and agrees thrombectomy likely to be beneficial. He talks with an interventionalist who carries out thrombectomies (most likely Interventional Neuroradiologist (INR) or Interventional Radiologist (IR) but might be from another specialty such as cardiology). The interventionalist agrees that thrombectomy is indicated and possible.
The two stroke physicians and the interventionalist share direct phone details to facilitate further communication between them.
The spoke team phone the SAS using the number agreed locally. Each region has a list of the numbers they should call supplied by SAS.
The SAS team estimate a 60 min drive time and immediately dispatch an emergency ambulance – in this case an air ambulance is not necessary. Please note that SAS will make the judgement on the most appropriate mode of transport.
NB: in some places the spoke consultant is asked to contact the INR/IR directly rather than going via the stroke physician. So please refer to your local pathway.

Vera is a 77yr old retired nurse who cares for her husband John who has dementia.
She got up at 8am, cooked John his breakfast but whilst tidying collapses with left sided weakness. She is unable to get up.
John presses their alarm, and their daughter phones to see what is wrong. John is clearly distressed so she drives around arriving at 9am. Finding her mother on the floor with left facial droop and unable to get up she phones 999 at 9.10am.
At 9.30am the paramedics arrive, diagnose a probable stroke (+ve FAST test, normal BM, BP 165/80). They take Vera to the nearest emergency dept, pre-alerting them when about 10 mins away.

Paramedics arrive in Resus with Vera at 9.50am

The paramedics hand over the patient, reporting that they were called at 9.10am and arrived at 9.30.am. The ED team quickly assess Vera who appears unaware of her severe left hemiparesis. Although she can talk and remembers falling she cannot tell them when this happened.
Fortunately, Vera’s daughter arrives and can confirm that her mother must have been OK after waking because she had cooked her husband John his porridge.
Therefore, it was clear that the onset was probably between 8 and 9am and therefore thrombolysis and/or thrombectomy are treatment options. Her daughter is given written information re hyperacute care.
- After stroke, hallucinations are usually visual.
- It is difficult to know how many people experience hallucinations as they are under-reported due to the association with mental illness.
- Hallucinations range from people seeing simple shapes and colours to complex scenes (Charles Bonnet syndrome). Ref: De Haan, Edward H.; Nys, Gudrun M.; van Zandvoort, Martine J.; Ramsey, Nick F. The physiological basis of visual hallucinations after damage to the primary visual cortex, NeuroReport: July 16, 2007 -Volume 18 – Issue 11 – p 1177-1180 doi:10.1097/ WNR.0b013e32820049d3
- Hallucinations are associated with damage to the occipital lobe or the brainstem and thalamic areas of the brain.
- Stroke patients are usually aware that their hallucinations are not real.
- Three theories try to explain why hallucinations happen after stroke:
- the damaged areas of the occipital lobes no longer inhibit the undamaged areas resulting in increased visual activity
- there is increased firing of neurons from the scar tissue of damaged areas
- there is less competition from damaged areas of the brain which reduces the threshold from which hallucinations can happen
- Hallucinations usually fade after several weeks.
Links to further reading:
Charles Bonnet leaflet [PDF, 27KB] (with permission of the British & Irish Orthoptic Society)
Esme’s umbrella
This animation shows the risks of stroke after a TIA/stroke in people not treated (top – red men) and treated (bottom – orange men) with medications (combination of antiplatelet, blood pressure and cholesterol lowering drugs). The boxes at the bottom show the difference in the number of patients having a stroke i.e. the number of strokes which would be prevented if 100 patients were treated over different time periods.
The risk of stroke in this group of patients in the first year is only 18% – compared with 25% for the “average” patient (as per previous animation) because this group excludes those patients with atrial fibrillation and carotid stenosis who have a higher than average risk of stroke.
The combination of antiplatelet treatment, statins and blood pressure lowering will reduce the risks by nearly half e.g. 18% to 10% in the first year, so if one treats 100 patients 8 of them will avoid a stroke in the first year because of the treatment. The number of people avoiding strokes gradually accumulates over time.
For more information on AF and CHADS2 & CHA₂DS₂-VASc score (stroke risk calculator) visit Topic Loop: Atrial Fibrillation.