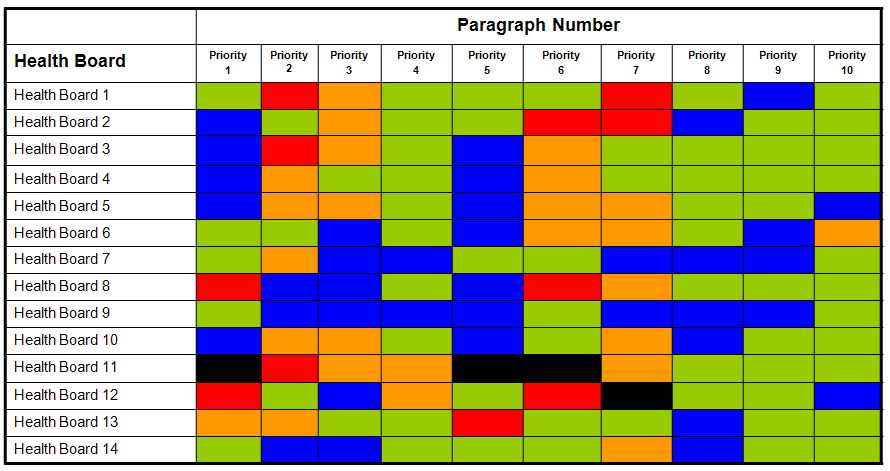
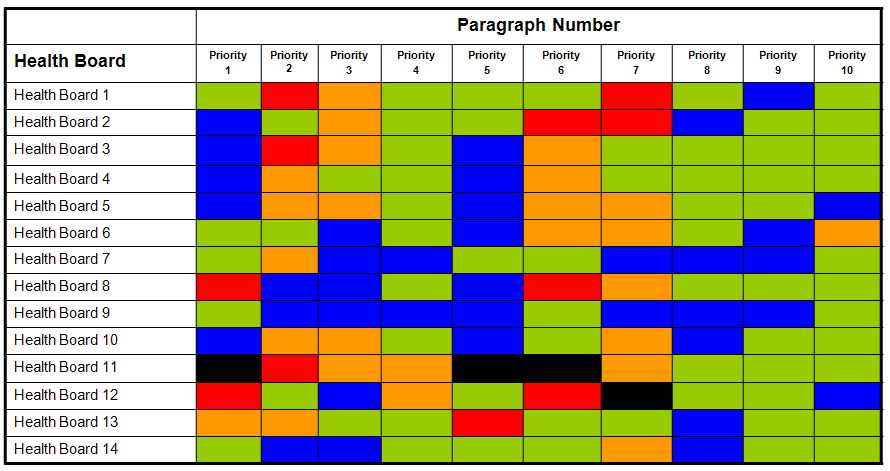
The table below shows each of the 14 NHS Boards in Scotland and how they are performing against the current top 10 priorities from the Better Heart Disease and Stroke Care Action Plan agreed by the National MCN Managers group and endorsed by the National Advisory Committee for Stroke at the Scottish Government.
The priorities may change over time as progress is made. Some examples of priorities are given in the additional information box.
The different colours denote each Board’s progress with the priority (see colour key under the table and an example of how these are defined for one of the priorities on the next page.)
The National Advisory Committee for Stroke (NACS) set out a plan to deliver key actions from the BHD&SC Action Plan.
MCN Managers in each Health Board will lead delivery of the key actions.
Ten priority areas have been agreed by the National MCN Managers Group (and endorsed by NACS) and performance against these key performance indicators are monitored by the National Action Plan Co-ordinator and Stroke MCNs across Scotland.
Priority areas are reviewed during visits to the NHS Boards by the National Action Plan Coordinator.
Local Action Plans to improve performance in individual Board areas are agreed locally by Stroke MCNs.
Better Heart Disease and Stroke Care Action Plan (2009) (BHD&SC Action Plan)
This action plan reflects the direction set out in Better Health Better Care: Action Plan in the way it seeks to respond to a series of challenges:
- Listening to what people with, or at risk of heart disease or who have had a stroke tell us about the kind of services they want
- Responding to developments in the evidence base, as reflected in the suite of SIGN Guidelines on CHD and cardiovascular disease (CVD) published in February 2007, and revised stroke guideline published in December 2008
- Introducing a new focus on prevention of ill health through anticipatory care approaches
- Reducing health inequalities across Scotland
- Meeting the needs of increasing numbers of older people and
- Responding to changes in our workforce
The Healthcare Quality Strategy sets out the Scottish Government’s intention to build on the collaborative, cross-disciplinary working exemplified by MCNs, as a well established approach to supporting and delivering high-quality healthcare. The Chief Executive Letter (CEL) 29 (July 2012) also notes that networks are ideally suited to delivering service redesign, quality improvement, strategy and planning across pathways working across boundaries of departments, teams, units, sectors, agencies and Boards.
MCNs improve quality and efficiency of services to patients through consensus and collaboration, by enabling clinicians, patients and service managers to work together across boundaries to deliver safe, effective and person-centred care.
MCNs are also involved in:
- Helping NHS Boards to achieve national outcomes that can be measured by the national indicators and HEAT targets.
- Linking data outputs to the standards of delivery of clinical care.
- Delivering on priority actions from the Better Heart Disease and Stroke Care Action Plan [.pdf]
- Linking all of the above to locally developed action plans focussing on improvement in the delivery of stroke care in their local area.
Further general information on MCNs can be found at:
Scottish Government communications regarding Managed Clinical Networks
Managed Clinical Networks (MCNs) have been forming in every health board in Scotland since 1998. They are made up of a network of people whose shared interest is in one particular area of health. MCNs membership usually comprises healthcare professionals, patients and carers, health managers, colleagues from social care and voluntary organisations, e.g. CHSS or the Stroke Association.
Their role is to work together to:
- make recommendations about what local healthcare services are required
- make the best use of resources available to provide these
- ensure that standards of care are equal to those provided elsewhere in Scotland
Key areas of work for MCNs include:
- Patient involvement
- Social care
- Service planning
- Quality assurance programmes
- Clinical governance
- Funding arrangements
- Workforce arrangements
- Information Technology arrangements
- Evaluation arrangements
Introduction to Quality Improvement
Using the outputs of audit coupled with the evidence from research, guidelines and standards the stroke Managed Clinical Networks (MCNs) should develop an Action Plan to ensure service improvement in relation to the delivery of stroke care.
This is driven by the Healthcare Quality Strategy of NHS Scotland published in 2010.
“By establishing a shared understanding of quality and a commitment to place it at the heart of everything we do, the Quality Strategy represents a unique and important opportunity for all of us to work together to our mutual benefit to make our NHS even better, for now and in the future”
Ref: Scottish Government
References
Kaku, A, Lowenstein, D. (1990). Emergence of recreational drug abuse as a major risk
factor for stroke in young adults. Medicine, psychology annals of internal medicine. 113, pg 821-827.
Modi V, Singh A, Shirani J (October 07, 2021). Marijuana Use and Stress Cardiomyopathy in the Young. Cureus 13(10): e18575. DOI10.7759/cureus.18575
Links to further reading and resources
For advice for families of people who use drugs visit: NHS UK live well addiction support
For honest information about drugs visit: Talk to Frank
For Scottish Public Health Observatory illegal drug use health harm data visit: ScotPHO
Martinez-Majander, N. (2018). Illicit drug use and risk of stroke. European Stroke Organisation (ESO).
Nutt, D. (2020). New psychoactive substances: Pharmacology influencing UK practice, policy and the law. British Journal of Clinical Pharmacology. 86 (3), pg 445-451.
For information on reducing the risk of stroke and heart disease see: CHSS Essential Guide.
For essential support fort under 25s visit: The Mix
For more information on recreational drugs and alcohol visit: Mind
For more information on recreational drugs visit: Patient Info

Recreational drug use and association with stroke
The term recreational drugs refers to illegal and prescribed medications that are used inappropriately to produce a pleasurable or other effect that the user feels (initially) improves their quality of life or provides an (emotional) escape.
However a number of recreational drugs can significantly increase the risk of having a stroke. Abuse of these drugs should be considered in any person with stroke particularly younger persons, even if other risk factors are present and/or the person denies the use of drugs (Kaku & Lowenstein 1990).
The actual number of patients who present with stroke from use of drugs can be hard to quantify. It can be difficult to obtain an accurate case history regarding recreational drug use. Increasing numbers of people using recreational drugs and the increase in stroke in younger people (15-44 year olds) appear to be linked. In a study by Kaku and Lowenstein 1990, recreational drug abuse was the most commonly identified potential predisposing risk factor for stroke in patients less than 35 years old. (Kaku & Lowenstein 1990).
There are a number of drugs that may precipitate ischaemic or haemorrhagic strokes. Mechanisms include through raising blood pressure, introducing infection, heavy metal contamination of the drug, causing arrhythmias or direct effects of the drug. Examples include Cocaine, heroin, amphetamines, MDMA, ketamine and marijuana, all of which are illegal to possess.
Prescription drugs used inappropriately can also increase the risk of stroke. These include opioids, Gabapentinoids, antipsychotics, anticholinergics, which includes antihistamines, sleeping tablets and some antidepressants or antispasmodic medications. There are others including herbal and plant based products, such as Khat, Kratom and St. John’s Wort that have also been linked to ischaemic and haemorrhagic strokes.
NB: It is important to be aware that stroke can also be a recognised side effect associated with certain prescription medications. However a decision to start someone on such medication will have been weighed against the therapeutic benefit of the new drug. This risk information should be discussed between the person and their doctor, pharmacist or a specialist healthcare professional when commencing any new drug treatment.

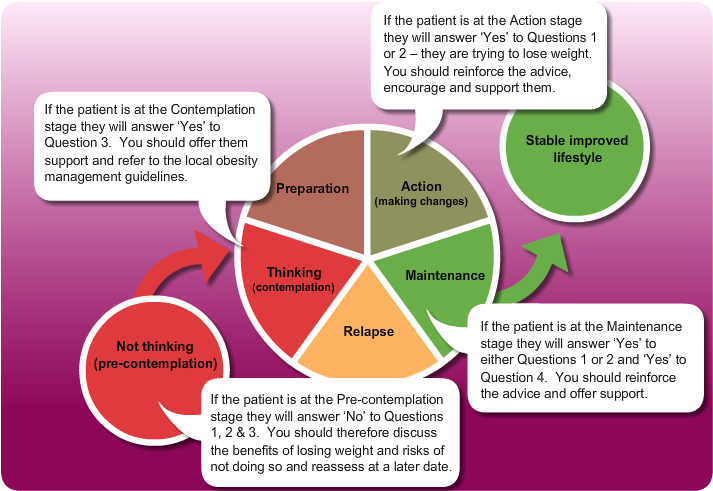
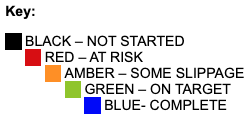
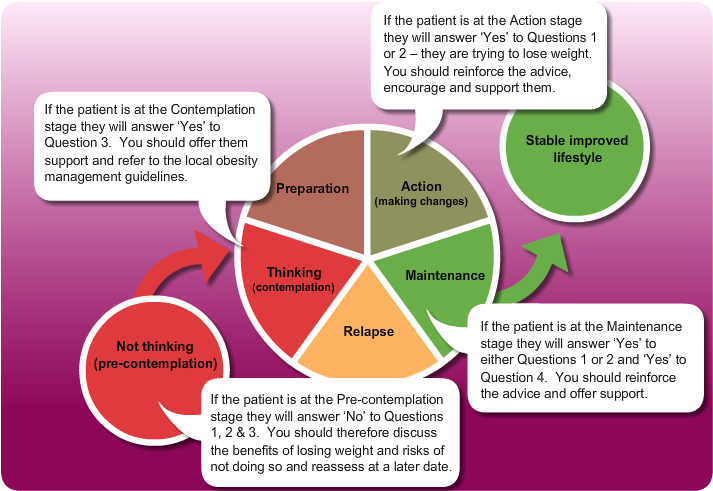
The Readiness to Change model can be used to assess if someone is ready to lose weight.
Questions to ask the patient
- In the past month, have you been actively trying to lose weight? Y/N
- In the past month, have you been actively trying to keep from gaining weight? Y/N
- Are you seriously considering trying to lose weight to reach your goal in the next 6 months? Y/N
- Have you maintained your desired weight for more than 6 months? Y/N