- Waist measurement is another way to determine fat distribution. Abdominal fat distribution increases the risk of developing heart disease, hypertension and Type 2 Diabetes.
- Waist circumference should be used as an additional measure in people with a BMI less than 35 kg/m2.
- Increased risk is identified in waist measurements over:
- 94cm – European men
- 90cm – Asian men
- 80cm – Women
Category: Advancing Modules
BMI
- BMI is used as an indicator of health risk.
- Based on weight and height (weight in kg/height in m2) it categorises risk as follows:
| Healthy | 19 – 24.9 |
| Overweight | 25 – 29.9 |
| Obese | 30 – 39.9 |
| Morbidly obese | over 40 |
- BMI may not always be a good indicator of body fat as muscular people may have a high BMI but not a high fat level.
Assessing risk
It is important to recognise if a person has an increased risk of developing obesity.
The National Obesity Forum suggest the following measurements and investigations are carried out to assess risk:
- Body Mass Index (BMI) calculated using a person’s height and weight
- Waist circumference
- Blood Pressure
- Fasting blood glucose
- Fasting lipid profile
- Thyroid function
Health and weight
Introduction
- Obesity is a major public health concern in Scotland and levels continue to rise.
- Being overweight increases your risk of ischaemic stroke by 22% and being obese by 64%.
- The aim of a weight management plan is to achieve a weight loss of 0.5-1kg per week.
- This weight loss can be achieved by consuming a diet that has a 600 kcal/day deficit (an achievable and sustainable target).
- Weight management programmes should include advice on increasing physical activity that is appropriate and sustainable.
Key points about headache after stroke
- Occurs in nearly one quarter of patients with acute ischaemic stroke
- Generally worst on day of stroke onset
- Often on the same side as the stroke lesion
- More common in posterior circulation stroke
- Stronger association with younger age, female sex, and history of migraine
- Severity is not related to the size of the stroke lesion
- There is no association between headache and outcome
Some practical points for clinical practice
- The medication Modified Release Dipyridamole is used much less now but important to enquire about it since frequently causes headache
- Movement and cough can exacerbate headache after stroke
- It is important to exclude other stroke complications which can cause headache, notably arterial dissection
- It is useful to include possible headache as a specific question on admission to the acute stroke unit to ensure it is not overlooked
Headache after stroke

Overall prevalence 25 – 60%
- Ischaemic stroke 25 – 30%
- Haemorrhagic stroke 34 – 60%
Headache after stroke or TIA is often overlooked by clinicians as a result of concentrating on clinical signs and stroke management
Which strokes most commonly cause headaches?
More often associated with:
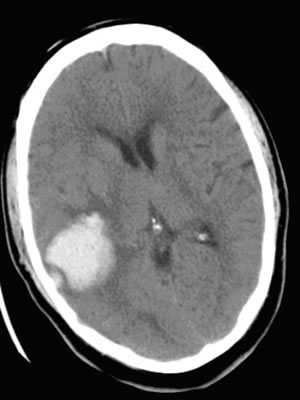
- Haemorrhage (see picture below) than infarct
- TIA than stroke
- Cortical than deep white matter strokes
- Thrombotic than embolic stroke
- Venous than arterial stroke
Approaches to treatment
Giant Cell Arteritis is usually treated with steroid medicine. Treatment should begin as soon as possible to prevent sight loss.
- High dose prednisilone (e.g. 60mg daily) for several weeks and then reduced over a period of years
- Unfortunately prednisilone will raise blood pressure and blood sugar and thus worsen the risk factor profile
- Antiplatelet drugs may reduce risk of embolism from damaged vessels – but may worsen indigestion caused by steroids
For more information on giant cell arteritis (temporal arteritis) visit NHS UK.
Assessment
Giant cell arteritis
Introduction
Giant cell arteritis:
- A disease which occurs in people over 50 yrs and more often much older – it is exceptionally rare in younger people
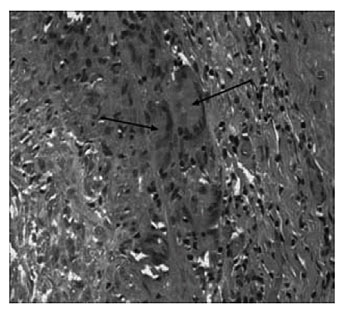
- Causes inflammation of medium sized arteries e.g. vertebral, carotid ophthalmic arteries – cause is unknown (see image below)
- May present suddenly with severe headache or stroke, or with a more chronic illness developing over weeks or even months
- Often affects the arteries in the head, particularly the temples, so can also be called Temporal Arteritis
- Inflammation may damage arteries causing them to block or clots form on damaged lining of the artery (intima) which can embolise to the brain or other organs
- Usually associated with a very high ESR – i.e. >60mm per hour
- It’s serious and needs urgent treatment
- Should be confirmed with a biopsy of an artery – most often the temporal artery – this can be done under local anaesthetic as a day case
- The biopsy will become uninformative within days of starting treatment so should be done early.
How are SIGN guidelines produced?
The Scottish Intercollegiate Guidelines Network (SIGN) develops evidence based clinical practice guidelines for the National Health Service (NHS) in Scotland.
Guidelines are usually written by a multidiciplinary group who will:
- Decide on questions/issues/scope
- Search for evidence
- Appraise evidence
- Write draft guideline
- Consult widely
- Write final guidelines
- Publish and disseminate widely
- Encourage use in everyday practice
Other organisations, including National Institute for Health and Clinical Excellence (NICE) and the Royal College of Physicians Intercollegiate Stroke Working Party produce evidence based guidelines in the UK.


