Local Development Plans are measures for NHS Scotland Health Boards. The plans are set each year after consultation with stakeholders and cover a variety of areas. Progress is measured throughout the year and NHS Boards are held to account during annual stroke care audit.
The main areas include:
- improving health and life expectancy
- continuously improving the effectiveness and efficiency of the NHS in Scotland
- recognising patients’ need for quicker and easier use of NHS services; and
- ensuring patients receive high quality services that meet their needs
What are the Clinical Standards for Stroke Care in Scotland?
Scottish Stroke Care Standards
NHS Quality Improvement Scotland (NHS QIS) produced clinical standards for Stroke Services in March 2004. Scotland’s action plan for health and wellbeing Better Health, Better Care highlighted stroke as a national clinical priority. These standards were revised in June 2009 following publication of SIGN 108 in December 2008.
The NHS QIS standards focus on those parameters which have the best evidence for having an effect on patient outcomes, e.g. stroke unit care, swallow screening, brain imaging, acute aspirin use, delays to assessment in specialist neurovascular clinics, delivery of thrombolysis and early carotid intervention.
In 2012 the National Advisory Committee for Stroke (NACS) at the Scottish Government the Scottish Stroke Care Audit (SSCA) Steering Committee reviewed the current NHS QIS Standards for Stroke Care (June 2009) in collaboration with Scottish Stroke Managed Clinical Networks (MCN) and colleagues in the wider Scottish stroke community.
The proposed Scottish Stroke Care Standards were agreed, and implemented on 1st January 2013. These standards are now reviewed on an annual basis.
The current Scottish Stroke Care Standards are available to access here. More details are available on the next page.
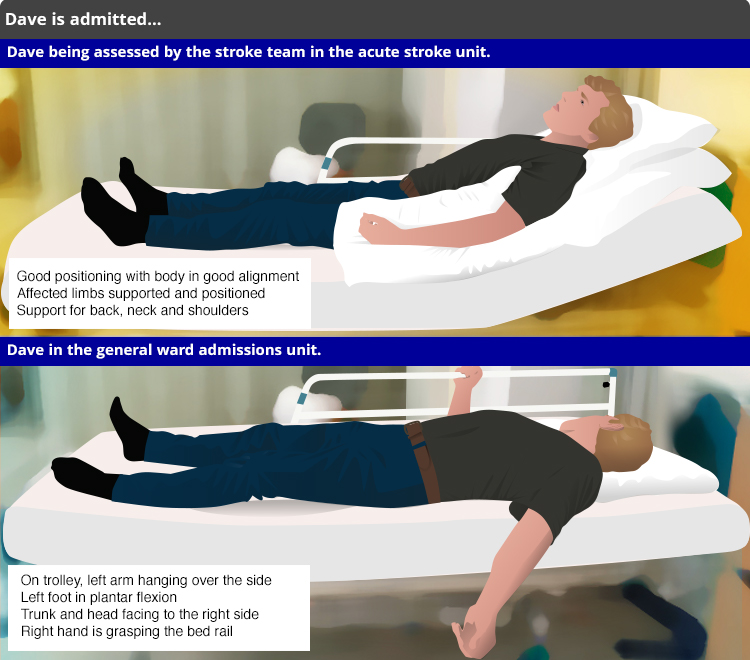
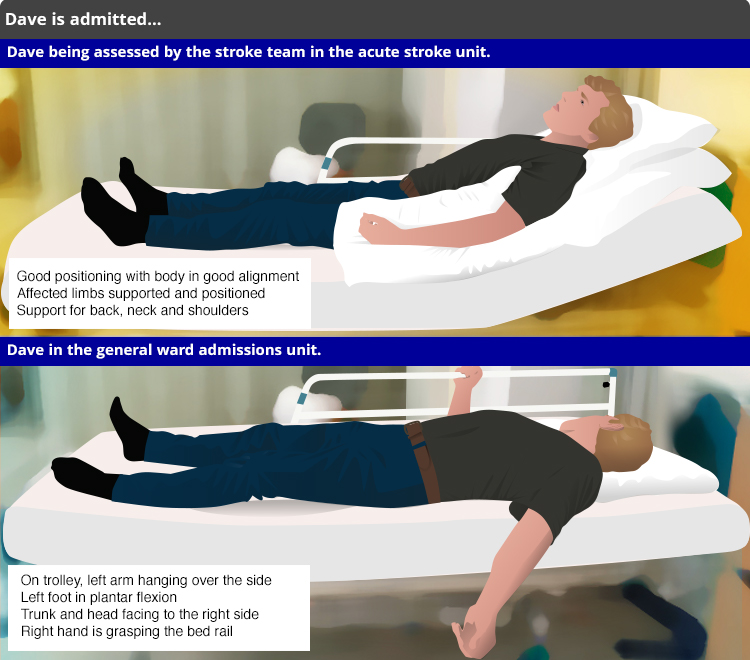
Dave is admitted on the Thursday before the long Easter weekend.
Monthly reports provide MCNs with up to date information on monthly and quarterly performance against the national standards for stroke care. They present 12 months of data on one chart in addition to the previous two years performance. This allows the MCNs to monitor trends in performance.
Monthly reports should be used locally to monitor current performance, highlight areas requiring improvement and influence change.
The annual national report contains information on individual hospitals, Board areas and Scotland as a whole. The annual national report is a public document. Again the MCNs disseminate to appropriate personnel within their Boards, e.g. Board members, ward teams and patient/ carer representatives. This document is also shared with the Scottish Government and Chief Executives within NHS Boards.
Further information regarding SSCA and previous copies of the annual national reports can be found at the Scottish Stroke Care Audit website.
What is the Scottish Stroke Care Audit (SSCA)?
The SSCA started collecting information about stroke care in 2002 and now includes all hospitals managing acute stroke in Scotland. Since its inception SSCA has helped to drive the improvements in stroke care which have contributed to the lower mortality rates and improved outcomes for stroke patients.
The SSCA collects a variety of information about stroke care however, the main purpose of the audit is to monitor performance against national standards and criteria.
Data are collected relating to the following groups of patients:
- Patients admitted to hospital with a stroke (inpatients)
- Patients seen in ambulatory care settings (TIA clinics, Emergency dept, Ward attendees)
- Patients receiving hyper-acute treatment with thrombolysis or thrombectomy
- Patients undergoing carotid intervention
Detailed criteria for assessing the quality and availability of stroke rehabilitation are available, and annual organisational audits determine whether comprehensive stroke services across the whole patient pathway are available in each NHS Board.
SSCA produces monthly and annual reports:
The monthly reports contain only information pertinent to individual Board areas. They are shared with stroke Managed Clinical Networks (MCNs) who disseminate them to appropriate personnel within their Boards, for example Board members, service managers, planners and ward teams.
What is Clinical Audit?
Clinical audit is the process used by health professionals to assess, evaluate and improve the care of patients in a systematic way in order to enhance their health and quality of life. It consists of four basic steps which are summarised in the diagram below:
Ref: Making Sense of Audit, D & S Irving, Radcliffe Medical Press, 1991, p16
After viewing the animation above, see if you can answer the questions below.

Dave is on his return from holiday
Dave Walker is a 39 year old man who works as a production manager in a food processing factory. On the Thursday before Easter he was well when he boarded his flight back from a holiday in America with his wife Jenny and their two sons aged 8 and 10. Jenny works part time as a teaching assistant. Dave woke up near the end of the flight with left sided weakness, altered feeling and slurred speech. On assessment he was found to have a dense left-sided weakness, marked left sensory loss and dysarthria. He smokes but has no other medical history.
In our case scenario we follow Dave in two different ways at the same time. This leads to different consequences and outcomes for muscle tone and spasticity in each version of Dave (Similar to the film Sliding Doors) One version of Dave goes to an acute stroke unit and the other Dave goes to a general ward. In both versions Dave is seen at the accident and emergency department.