Having completed this module you will have increased your knowledge regarding emotional lability, anxiety and depression post stroke.
Specifically you will have considered:
- How the emotional issues post stroke may adversely affect a person and their family. You will also have gained an insight into how emotional lability, anxiety and depression may affect a person’s rehabilitation and outcome post stroke.
- Why spiritual care is important and how you may support a person in a holistic manner, involving the multi-disciplinary team.
- The appropriate strategies available to support the diagnosis and treatment of emotional lability, anxiety and depression post stroke and how to gain access to these.
- The availability of resources, agencies and individuals that may be able to help a person and their family post stroke.
If Jennifer had not seen a reduction in her anxiety, a change to her treatment plan would be necessary. A number of options could be available including referring on to specialist mental health services. Many, but not all, Scottish Stroke MCNs have access to stroke-specialist clinical neuropsychology services and it may be appropriate to refer Jennifer to them or at least to consult with them in more detail over Jennifer’s treatment. Alternatively referring Jennifer to Older Adult Mental Health services that include psychiatrists, psychiatric nurses, clinical psychologists, and mental health OTs would be appropriate.
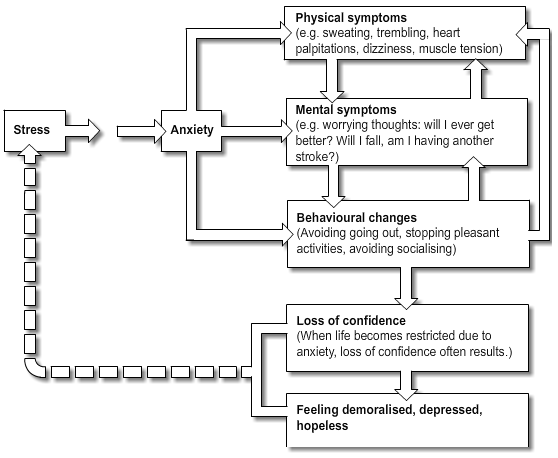
These professionals would work with Jennifer in more depth looking at factors that maintain and exacerbate her anxiety. Jennifer has already tried to increase her activity using a behavioural approach (i.e., looking to gradually increase her ability to go outside). If this had not been successful then specialist mental health professionals may focus more on her cognitions (e.g., her thoughts) surrounding her concerns about her physical ability, the likelihood of having another fall, and her health beliefs about having another stroke. They are likely to use cognitive behavioural therapy and focus on a here-and-now, problem-solving, goal-orientated approach looking to intervene at some of the stages shown in the diagram below that outlines what might be going on for Jennifer.
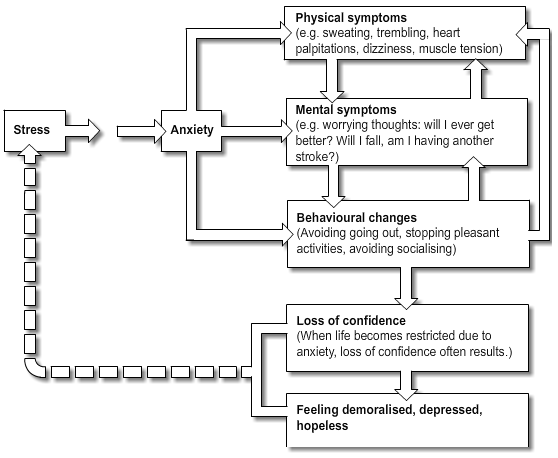
Diagram adapted from Powell, T. (2001). The Mental Health Handbook. Oxon: Speechmark Practical Photocopy Resource.
There is some (non Randomised Controlled Trials) evidence that psychological management can have a beneficial impact on fear of falling. Child, L., & Kneebone, I. (2002). Falls, fear of falling and psychological management. British Journal of Therapy and Rehabilitation, 9, 225-231.
Two months later Jennifer is still noticing improvements in her physical and emotional symptoms of anxiety as well as her ability to control these by using her chosen strategies. She no longer needs to use her diary as she is now aware of the triggers for her symptoms, however she regularly uses her diaphragmatic breathing exercises. Jennifer still feels that these are useful if she is going anywhere which is unfamiliar to her. By carrying these out it allows her to remain calm in most situations.
Jennifer has continued to set achievable goals which included walking to church alone. The goal setting strategy has proved to be beneficial and motivational for Jennifer. Jennifer’s daughter, her friends and the minister have all noticed an improvement in her mood and her confidence in her own abilities out with the home.
The stroke liaison nurse continues to follow up Jennifer’s progress and her recent mood screening test has shown continued improvement.
The nurse also gives Jennifer another HADS to complete. Select the following link to see the results of this: Jennifer’s HADS [PDF, 383 KB]
The nurse discusses these options with Jennifer. Jennifer would like to try to use goal setting and an anxiety diary. Together they develop a personalised goal setting plan. They try to focus on what Jennifer’s most important aims are and make the goals achievable. The nurse also explains to Jennifer how she may use her diary to chart when she has these feelings of anxiousness and what she is doing or planning on doing at the time they occur. The nurse also instructs Jennifer in effective diaphragmatic breathing techniques which some people find useful in helping them to relax. For further information on breathing techniques see the ‘Additional Information’ box below.
| Jennifer Parks 10th June: goal setting |
| Aim |
Goal |
Date to be achieved |
| Recognise triggers of anxiety |
Recognise triggers/effective use of diary/use rating scales 1-10 (10 indicating extreme anxiety) |
24th June (2 weeks) |
| Use diaphragmatic breathing technique at home when feelings of anxiety present. |
24th June (2 weeks) |
| Use diaphragmatic breathing technique outside the home if anxiety presents. |
2nd July (3 weeks) |
| Walking to church |
Gain confidence walking outside accompanied for 10 minutes. |
24th June (2 weeks) |
| Walk to church accompanied, 20 minute walk. |
2nd July (3 weeks) |
| Walk to church independently. |
10th July (one month) |
| Walk Tipsy her dog |
Walk Tipsy accompanied to the bus stop, 10 minute walk. |
24th June (2 weeks) |
| Walk Tipsy accompanied to the paper shop, 15 minute walk. |
2nd July (3 weeks) |
| Walk Tipsy unaccompanied to the paper shop. |
10th July (one month) |
| This goal setting plan will be reviewed on a regular basis. |
For more information about these common physical symptoms see the ‘Additional Information’ box below.
The nurse gives Jennifer a couple of useful booklets on emotional issues post stroke and tells Jennifer that she can discuss these with her in more detail at any time.
The nurse also asks Jennifer if she may complete another mood screening form so they can monitor her progress. Jennifer agrees and the nurse completes a HADS: Jennifer’s HADS [PDF, 203 KB]
For more information on the Hospital Anxiety and Depression Scale (HADS) view the ‘Additional Information’ box below.