During transfer, Joan is continually monitored for signs of deterioration. Prior to arrival at the interventional centre her condition deteriorates.
Transfer of patients to interventional centres
Two randomised trials have confirmed that emergency transfer of patients to interventional centres for PCI can be undertaken safely. Prompt transfer of patients for primary PCI was associated with a reduction in the end point of death, re-infarction and stroke at 30 days when compared to thrombolysis.
For more information see SIGN 148 PDF.
All of these contraindications need to be reviewed in the context of the clinical presentation.
For further information on the use of tenecteplase see: electronic Medicines Compendium (eMC)
Thrombolysis involves an injection of clot busting drugs (e.g tenecteplase), which are given directly into the vein.
Thrombolysis treatment may be an emergency treatment if PCI is not available. Treatment with thrombolysis is most effective when it is given as soon as possible. This helps to reduce damage to the myocardium and reduce the risk of complications. It may be administered by paramedics or GPs if transfer to hospital would delay treatment.
This treatment is not suitable for everyone as there is a risk of bleeding.
A standard treatment regime would be:
- Unfractionated heparin (5000 units IV)
- Tenecteplase (100 units per kilo IV)
Thrombolysis can also be given to reperfuse the brain after a stroke. For more information about thrombolysis in the treatment of stroke refer to: Stroke Training and Awareness Resources (STARs).
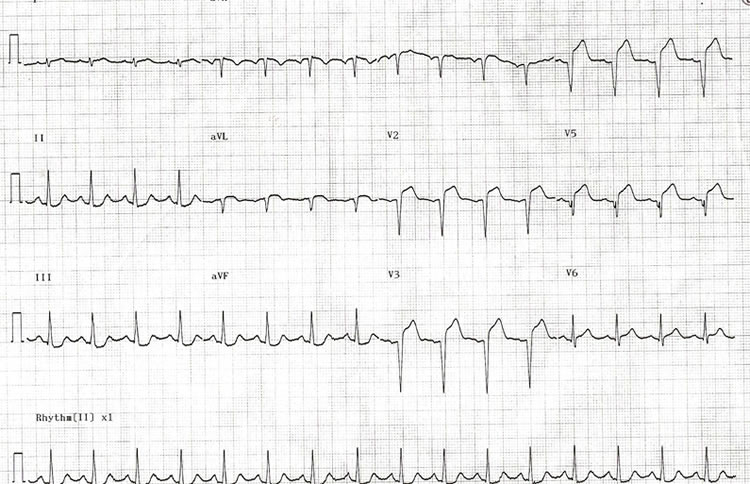
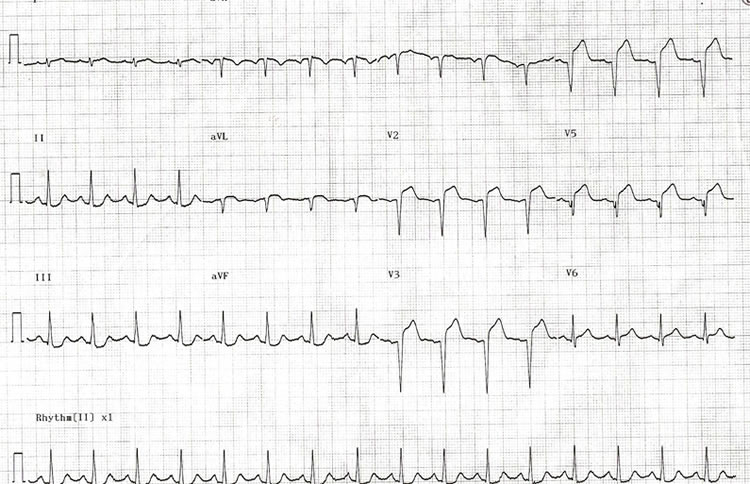
Based on initial Electrocardiogram (ECG) and clinical presentation, Joan is diagnosed with an anterior ST Elevation Myocardial Infarction (STEMI). Her case is discussed with an interventional cardiologist who feels that the time delay involved in her transfer to the interventional centre is too long for primary angioplasty. He recommends that she receives thrombolysis if there are no contraindications and transfer for assessment for Percutaneous Coronary Intervention (PCI) thereafter.
Joan is admitted to the emergency department after 5 hours crushing chest pain at rest.

 Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.
Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.
After a long journey they both decide on an early night. Joan is wakened at 5am by a crushing pain in the centre of her chest. She has never experienced anything like it before, and feels short of breath and nauseated. She does not want to alarm Mark but after 2 hours she wakens him as she is no better and starting to feel very frightened. Mark notices that Joan is clammy to touch and is concerned, he wants to ring for an ambulance but Joan refuses as she does not want any fuss. Mark finds an information pack in the cottage with details of the local community hospital and Mark drives her there. Joan vomits on her arrival at the hospital.

 Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.
Joan is a 42-year old Lawyer who lives in the west end of Glasgow with her partner Mark. She has been busy with a major court case working long days and weekends. Mark has been worried about Joan’s stress levels and arranges a surprise week at a cottage in the Highlands to help Joan unwind following the conclusion of the case. Mark has requested non-smoking accommodation as neither of them smoke. He has brought all of Joan’s favourite healthy foods and a few of her favourite wines. Joan is careful about her diet as she has risk factors for cardiovascular disease with her father having a myocardial infarction aged 55 and her mother suffering from high cholesterol and high blood pressure. Mark is aware that Joan has not been eating very well over the last few months and is looking forward to the break and spending some quality time together.