Aim
To increase knowledge and understanding of inherited cardiac disease and congenital cardiac disease
Inherited heart disease
After completing the module, you will be able to:
- describe the two main inherited cardiac conditions (cardiomyopathies and channelopathies)
- describe the signs and symptoms of inherited cardiac disease
- identify when inherited cardiac disease should be considered as a diagnosis
- recognise the complications that may arise from inherited cardiac disease
- understand the role of specialist multidisciplinary clinics
- discuss management pathways for patients with inherited cardiac disease
- explore person centred approaches specific to living with inherited cardiac disease, across the lifespan
Congenital cardiac disease
After completing the module, you will be able to:
- recognise the common presentations of congenital cardiac disease
- outline common investigations for congenital cardiac disease
- demonstrate awareness of endocarditis prevention
- be aware of potential management options for patients with congenital cardiac disease
- recognise the potential requirement of some patients with congenital cardiac disease for lifelong specialist care
- explore person centred approaches specific to living with congenital cardiac disease, across the lifespan

Module Team
Group Members
Zanna Christie, Arrhythmia Specialist Nurse, NHS Tayside
Anna Choy, Consultant Cardiologist (Familial Arrhythmia Network Scotland lead), NHS Tayside
Muhammad Walayat, Consultant Paediatrician, NHS Lothian
Sandra Jansz, Nurse Practitioner, Scottish Adult Congenital Cardiac Service
Contributors
Lynn Miller, Consultant Cardiologist, NHS Fife
Hazel Hailey, Principal Genetic Counsellor, NHS Grampian
Elaine Muirhead, Nurse Practitioner, Scottish Adult Congenital Cardiac Service
Reviewers
Niki Walker, Consultant Cardiologist, Scottish Adult Congenital Cardiac Service
Karen Smith, Nurse Consultant, Cardiology, NHS Tayside
Learning outcomes
- Describe the two main inherited cardiac conditions (cardiomyopathies and channelopathies)
- Describe the signs and symptoms of inherited cardiac disease
- Identify when inherited cardiac disease should be considered as a diagnosis
- Recognise the complications that may arise from inherited cardiac disease
- Understand the role of specialist multidisciplinary clinics
- Discuss management pathways for patients with inherited cardiac disease
- Explore person centred approaches specific to living with inherited cardiac disease, across the lifespan
General Medical Disclaimer: The information, including but not limited to, text, graphics, images, recommendations, opinions and other material contained on or accessed through this website (or in any module or content accessible through this website) (together “Website”), is intended for general informational purposes only. The information should not be considered as professional medical advice, diagnosis, recommendations or treatment. The information on this Website is provided without any assurance, representations or warranties, express or implied. We do not warrant that the information on this Website is applicable to all healthcare practices, geographical locations, health needs or circumstances. We do not warrant that the information on this module is complete, true, accurate, up-to-date, or non-misleading. You should always seek the guidance of a qualified healthcare professional before making any decisions related to your health or wellbeing. Never disregard or delay seeking medical advice due to something you have read on this Website. The use of or any reliance placed on any information provided on or accessed through this Website is solely at your own risk. If you have any specific questions or concerns about your health, please consult a qualified healthcare provider or other qualified medical professional. Do not rely on the information on this Website as an alternative to medical advice from your doctor or other qualified professional healthcare professional or healthcare provider.

This is the module test for ‘HEARTe 10. Hypertension’. It is strongly recommended that you work through the learning materials of the module prior to commencing this test. By going straight to the test you may miss out on valuable learning contained within the module. The answers to all the test questions are contained within the module. This information may have been provided in the ‘Additional Information’ boxes on some of the pages.
There are 10 questions and you must answer all of these correctly to obtain a certificate of completion.
You should allow approximately 10 minutes to complete the test.
Following further discussion, Ronnie and the practice nurse agree a way forward. The nurse writes this up in her notes, which include:
- Ronnie agrees to take amlodipine as it is prescribed once per day in the morning, making it easiest to remember.
- Ronnie will have a return appointment in two weeks to have his BP re-checked. In the meantime, Ronnie will keep a diary of when he’s is taking his tablets.
After the consultation with Ronnie, the nurse reflects on how the discussion went. Reflecting on practice can help nurses make sense of their work and, ultimately, improve care. The nurse decides not to address any lifestyle interventions at this stage. Instead, her focus is on building a therapeutic relationship with Ronnie.
Please enable JavaScript in your browser to see this interactive content.
Pulse point
You will find further useful information on reflection on the NMC website.
The nurse calls Ronnie in for his appointment
Please enable JavaScript in your browser to see this interactive content.
Non concordance can be divided into 2 separate underlying causes.
1. Intentional non-concordance.
This is where patient’s beliefs mean they make a conscious decision to not take their medications. It is important that health care professionals allow patients to express their beliefs in a non-judgemental environment. Some possible reasons for intentional non concordance are:
- Belief that medicines are no longer required.
- People can believe that long term making mediation can be harmful to their health as it develops dependency or build-up of the drug in heir system.
2. Non-intentional-non-concordance
This can be when:
- People forget
- They are too busy
- Or they stop for a period of time due to other factors, for example, family stress.
In order to suitably address non-concordance it is essential to fully explore and understand the reasons for it. Such discussions can often lead to the development of trust and respect between the patient and the health care professional.
While the practice nurse is reviewing Ronnie’s notes, he sits in the waiting room, worrying about how the appointment will go.
Please enable JavaScript in your browser to see this interactive content.
Ronnie fails to attend his last two annual hypertension review appointments and has not attended for his flu jab. The practice nurse notices this and phones to arrange a time that is suitable for Ronnie to attend. She reviews Ronnie’s notes before he comes in to the room for his appointment.
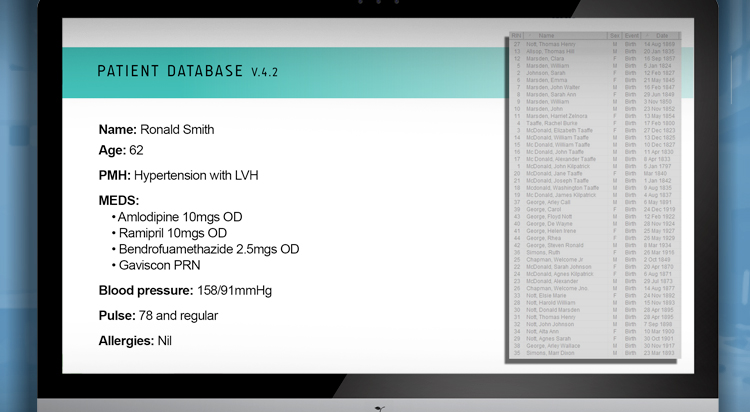
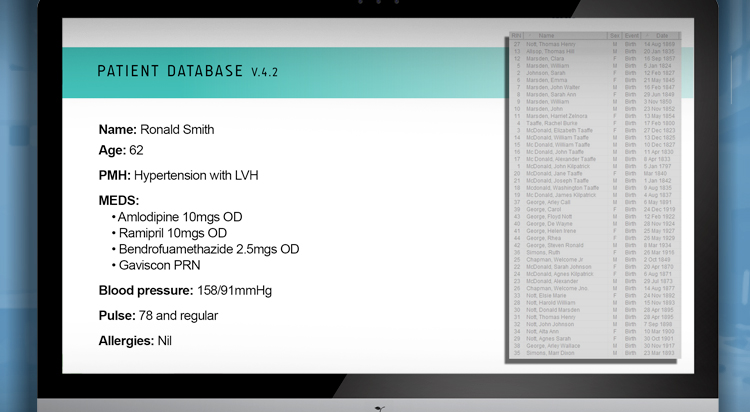
The practice nurse notices that Ronnie’s blood pressure is not within target, despite him being prescribed 3 antihypertensive medications.
One possible conclusion is that he has resistant hypertension.
This occurs in approximately 1% of people with hypertension. In resistant hypertension, it is essential that they are referred to secondary care for further review. However, before assuming that this is resistant hypertension, it is important to go back to basics and review Ronnie, ensuring that all tests and investigations have been carried out.
Secondary Hypertension NICE Guidelines

Meet Ronnie
Ronnie is 62 years old and works as a nightshift security guard three nights a week. He was diagnosed with stage 2 hypertension five years ago. At that time he was found to have left ventricular hypertrophy. A blood pressure review is carried out by his practice nurse every year.
Please enable JavaScript in your browser to see this interactive content.

Six months after starting medication, Evelyn is feeling well. She and her husband go walking every day, she takes her tablets as prescribed and she tries to maintain a healthy diet.
Evelyn will continue to be followed up annually at her GP surgery. After reading the information that was given to her, she now understands her condition better and the importance of taking her medication. She recognises how the lifestyle changes she is making help to maintain her BP and reduce her risk of CVD.