Hypertension is divided into two forms:
- Primary (or essential) hypertension (95% of people)
- Secondary hypertension
Primary Hypertension
- Primary hypertension has no single known cause but several mechanisms are linked to altered pathways in BP control. These are genetic factors, diet especially increased salt (sodium chloride) intake, obesity, insulin resistance, endothelial dysfunction, chronic excess alcohol, ageing, stress and sedentary lifestyle.
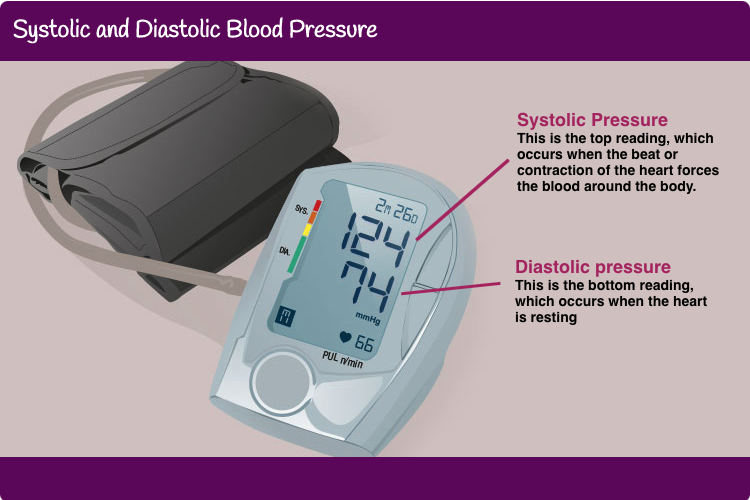
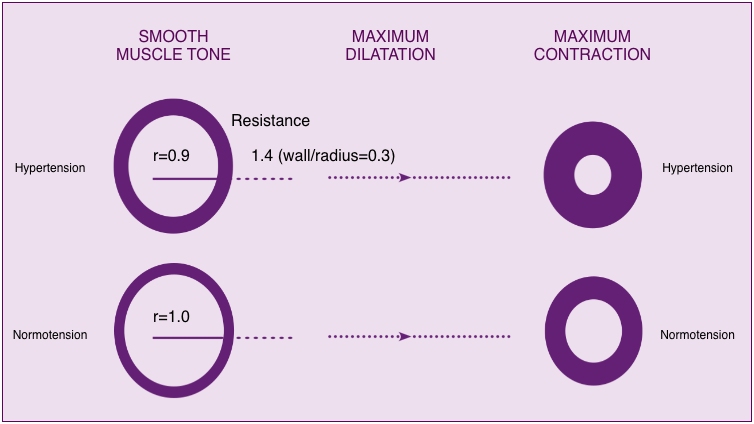
- The pressure against the blood vessel walls is affected by cardiac output and peripheral resistance. Altered pathways in BP control leads to sustained constriction of the arterioles (microscopic blood vessels in the circulation) resulting in increased peripheral resistance in the blood vessels. As the heart continues to pump normally, the pressure in the whole arterial system rises. This normally has no outward symptoms for the individual, unless very high.
Constricted, stiff arteriole vessel walls lead to increased pressure from blood flow within the arterioles
The increased pressure of blood flow against the artery wall leads to damage, resulting in atherosclerotic plaque formation. Signs of prolonged or severe hypertension can be found in target organ damage in the eyes, left ventricle, and kidneys. Presence of target organ damage increases the risk of vascular morbidity and mortality, and the need for treatment to lower blood pressure.
Secondary Hypertension
- In secondary hypertension BP is raised due to a known underlying cause:
- Renal disorders (e.g. chronic pyelonephritis, diabetic nephropathy).
- Vascular disorders (e.g. coarctation of the aorta).
- Endocrine disorders (e.g. primary hyperaldosteronism).
- Drugs (e.g. alcohol, cocaine)
- Miscellaneous causes (e.g. scleroderma, obstructive sleep apnoea).
- A search for secondary hypertension is only suggested by history, physical examination or routine tests indicate abnormalities.
- Investigations for secondary hypertension are not cost effective.