Why use 12 lead?
A 12-lead ECG is an important tool in clinical decision making and can provide a wealth of information, for example, diagnosis of evolving MI; identify potentially life threatening arrhythmias; long term effects of sustained hypertension; or acute effects of a pulmonary embolus. In contrast to cardiac monitoring, the 12-lead ECG shows the 3-dimensional electrical activity of the heart recorded from 12 different leads or viewpoints. It provides the whole picture. This is achieved by using Bipolar (I, II & III) and Unipolar leads (augmented leads & precordial chest leads).
ECG electrodes are placed on specific areas of the body in predetermined positions so that different pictures of the heart’s electrical activity can be recorded accurately and replicated between recordings.
The bipolar limb leads show the electrical differences between the positive and negative electrodes placed on the limbs as far away from the heart as possible. These 3 leads are equidistant from the heart and create an equilateral triangle (Einthovens triangle) which the heart sits in the centre of.
- Lead 1 shows the electrical difference between the left arm (positive electrode) and the right arm (negative electrode)
- Lead 2 shows the electrical difference between right arm (negative electrode) and left foot (positive electrode)
- Lead 3 shows the electrical difference between the left arm (negative electrode) and left foot (positive electrode)
Please enable JavaScript in your browser to see this interactive content.
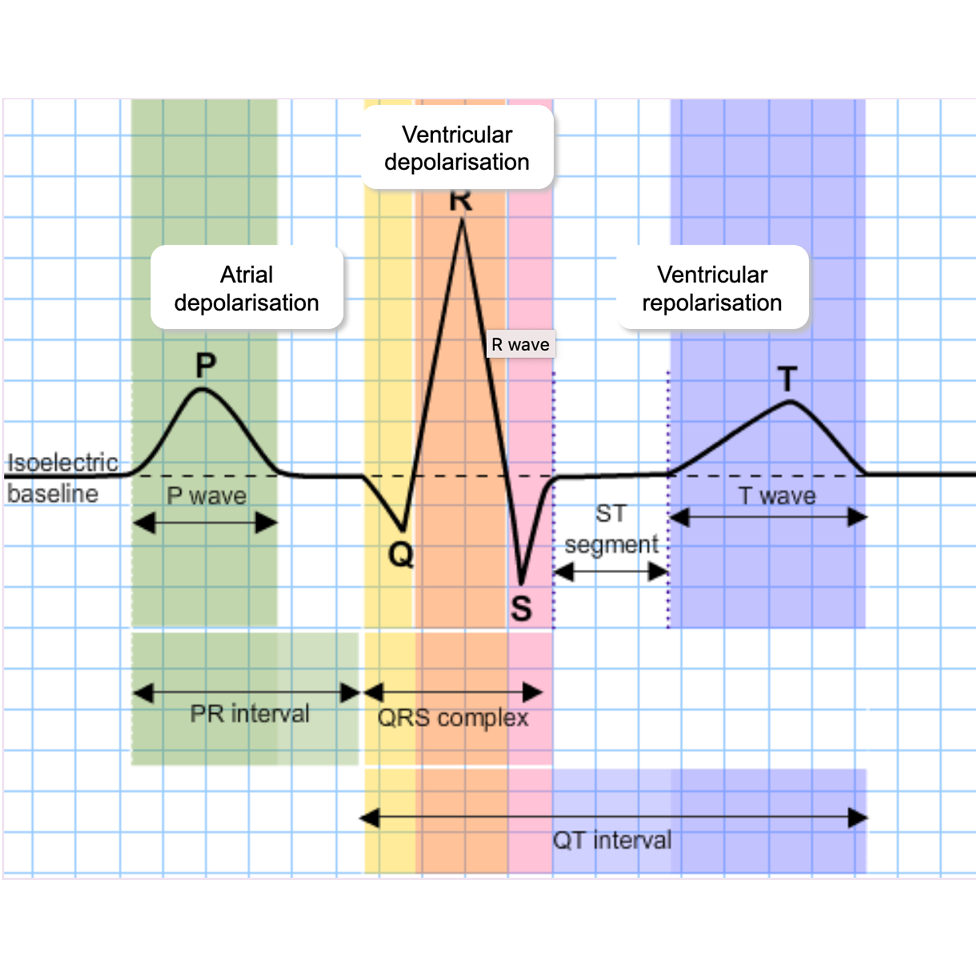
The Normal 12 lead ECG
When looking at an ECG its important to know what is normal.
Within the first 6 leads (I,II,III, avR, avL and avF) all, with the exception of aVR, should be upright.
In the precordial or chest leads the r wave progresses from small to tall from V1 to V6
The polarity or direction of the ST segment and T wave are generally the same as the preceding QRS complex, for example, if the QRS complex is positive or upright then the T wave will also be positive.
All ST segments should remain on the isoelectric line or baseline.
Please enable JavaScript in your browser to see this interactive content.
See Common Cardiac Investigations: The Electrocardiogram (ECG) for a video from Glasgow University on indications, equipment, placement, preparation and procedure and recording an ECG.