The blood results were all normal, the echocardiogram was normal and showed no structural abnormalities. A 24-hour Holter monitor showed an episode of AF. This episode coincided with Dillon’s diary entry when he had his symptoms.
Below is a copy of his 12 lead ECG which captured his AF.
Note the rhythm is irregular and there are no clear P waves.
Below there is a section of ECG chart without the green highlight points, if you wish to cross-reference it with the interactive chart underneath:
Dillon’s diagnosis is paroxysmal AF. At this stage the GP may decide to refer on to local cardiology department. Check your local policy for the correct referral pathway.
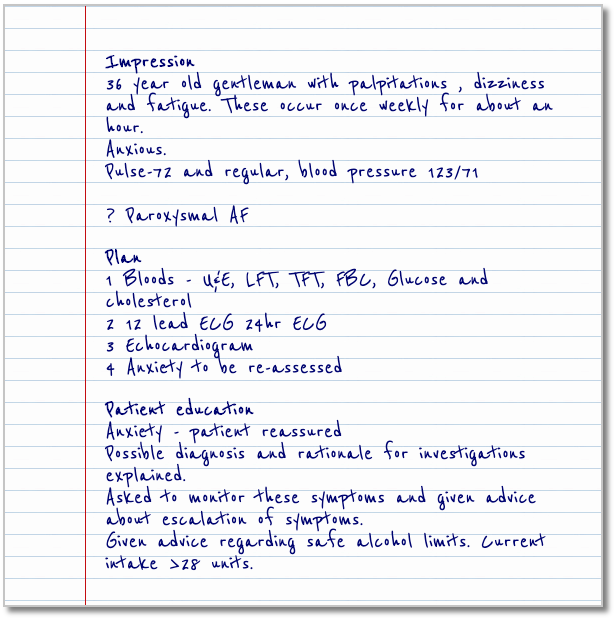
Dillon has been telling his GP about his new symptoms. The GP suspects the symptoms may be due to AF and so uses a focused approach to establish Dillon’s symptoms.

Meet Dillon
Dillon is a 36 year old man who has been experiencing palpitations. They usually last about an hour at a time and in the last month have occurred at least once weekly.
Dillon works as a senior police officer which he finds rather stressful at times.
Watch the video below to see an example of how a score calculator can be used to assess a patient’s risk. See the link underneath for an example of online calculators available to you.
CHADS2 calculator (3rd party website recommended by NHS Greater Glasgow & Clyde)
CHA2DS2-VASc calculator
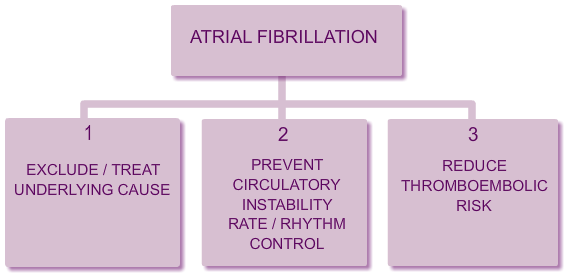
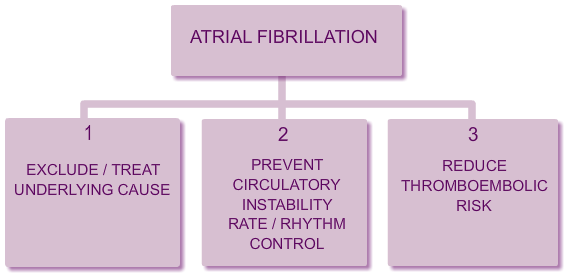
1. Exclude/treat underlying causes.
In all people with AF it is important to assess for treatable causes. Depending on the potential underlying cause, consider referral to appropriate specialist, according to local guidelines or pathways.
2. Cardiac stability.
In order to prevent further cardiac complications, it is important that everyone’s heart rate is controlled to approx less than 100bpm and that they are no longer symptomatic of the AF.
3. Stroke risk.
As soon as a diagnosis of AF is confirmed, all patients must have their stroke risk formally assessed and acted upon.
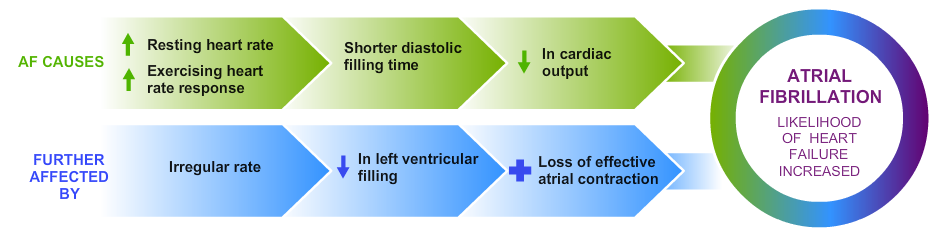
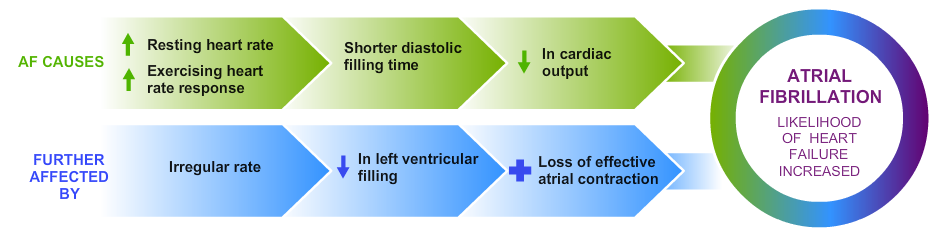
The long-term consequences of atrial fibrillation and heart failure can be similar to the “chicken and egg” theory as it’s often challenging to specify which came first.
The relationship between the two is only partly understood and there are many studies ongoing into this area. Certainly, one precipitates the other. So if you have AF you are more likely to develop HF and if you have HF you are more likely to develop AF. This could be due to:
- Common risk factors (I.e. hypertension, obesity, diabetes, age etc)
- Common cardiac conditions (valvular disease, ischaemia heart disease and structural heart disease).
These two things combined with a little science (myocardial and extra – cellular changes along with some electrophysiological and neurohormonal changes) create an environment which is predisposed to the development of both atrial fibrillation and heart failure.
The majority of patients diagnosed with AF will be reasonably well and suitable to be managed within primary care, however some patients will present acutely unwell with AF – these patients will have a heart rate greater than 160bpm and may be hypotensive. Their symptoms will be new onset (less than 48hrs) and they will experience some or all of the following symptoms:
- Breathless
- Palpitations
- Dizziness or syncope
- Signs of acute heart failure
- Chest pain
- Fatigue
These patients should be admitted acutely to hospital.