AF is classified by a patient’s history and the duration of AF. Many patients, about 1 in 5, have no symptoms of AF and so their AF history is unknown. The diagram below shows the different classifications of AF. It is important to remember for most people this is a journey that may progress. Both the clinician and the patient should be aware of this when making the initial diagnosis and planning long term management and review.
Category: HEARTe
Common causes of AF
Incidence and prevalence of AF
ESC (2012) suggests the current estimate of the prevalence of atrial fibrillation (AF) in the developed world is approximately 1.5–2% of the general population, with the average age of patients with this condition steadily rising, such that it now averages between 75 and 85 years.
One in four people aged over 40 will experience AF (The Framingham Heart Study, 2004). The incidence of AF doubles every decade after the age of 55 years. A recent study predicted an increase in the prevelence of AF in the general population by 2050 to 5%.
Consider this map which shows the ISD Scotland Quality Outcomes Framework (QOF) reported prevalence of atrial fibrillation in Scotland 2012/13.
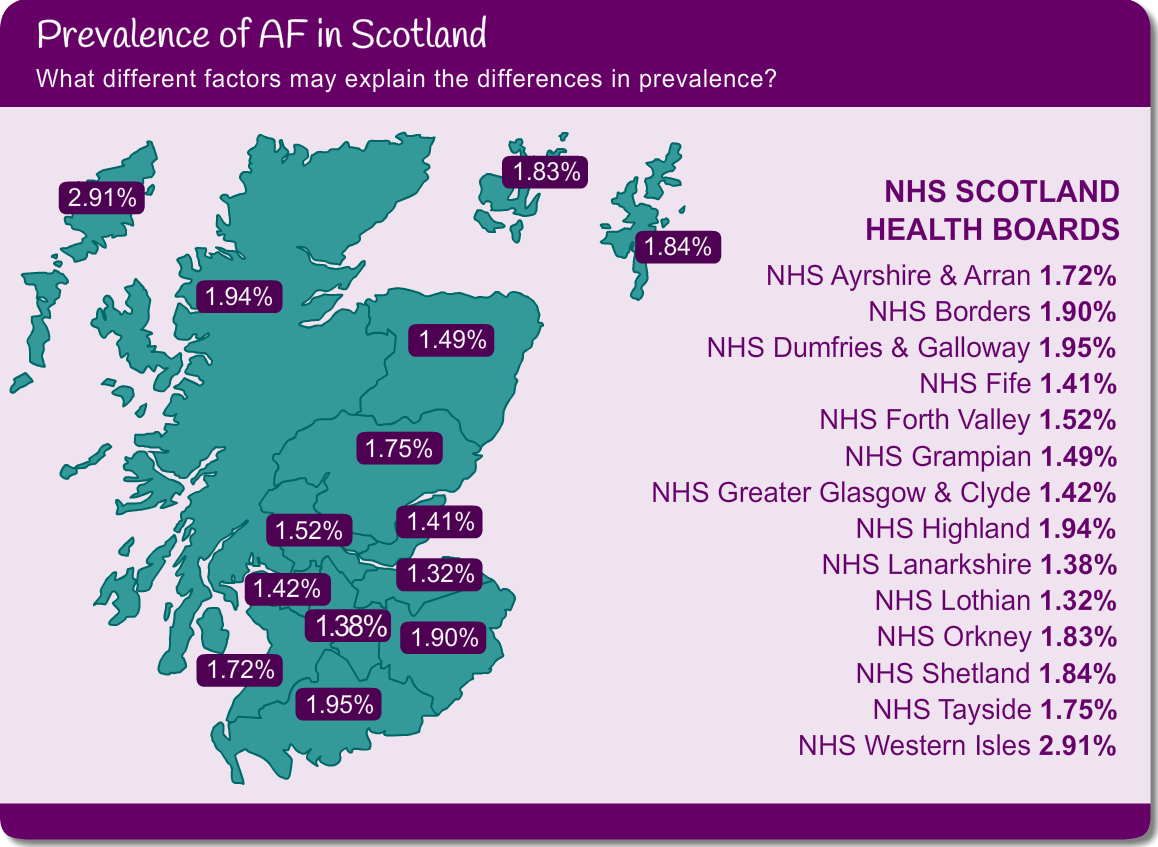
Some things you may want to consider:
- prevalence in more affluent areas
- increase in survival
- increase in health screening
Atrial Fibrillation (AF)
Atrial fibrillation is the most common sustained cardiac arrrhythmia. It is defined as:
- The surface electrocardiogram (ECG) shows “absolutely” irregular QRS complex intervals
- There are no distinct P waves on the surface ECG
This module is only covering the management of atrial fibrillation and not atrial flutter. However the stroke risk for both these arrhythmias are similar and the stroke risk stratification tools can be used for both.
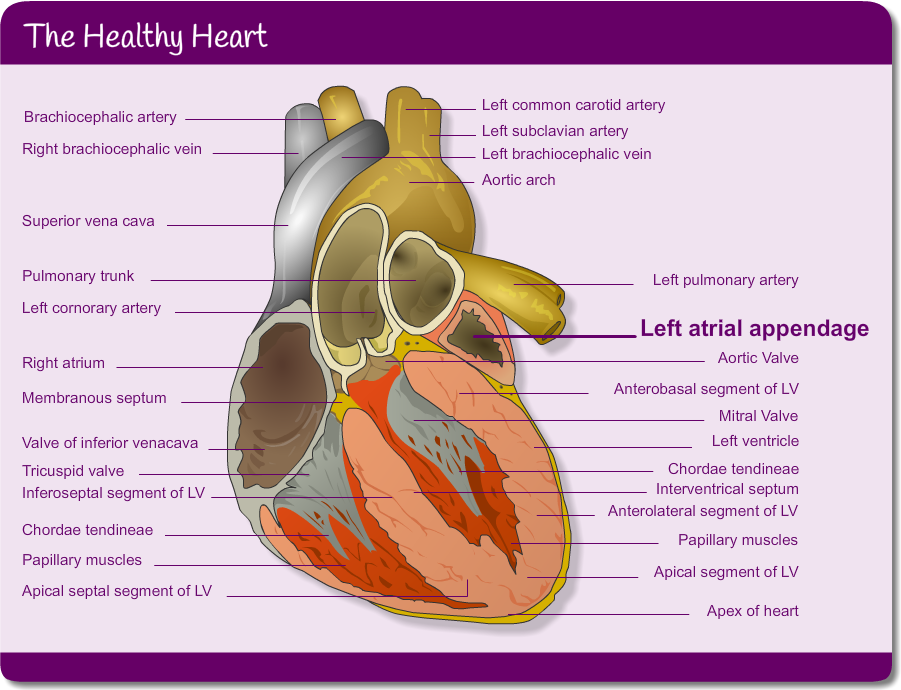
The healthy heart
Before continuing with the atrial fibrillation module we recommend that you complete the learning outcomes and assessment of module 1: Healthy Heart & Investigations. You should pay particular attention to the pages relating to normal cardiac conduction pathways.
In people with AF the left atrial appendage which sits adjacent to the left atrium, is clinically important. Have a look at more detailed physiology in the picture below. In AF the development of thrombus usually takes place in the left atrial appendage due to its position.
Learning outcomes
On completion of this module you will be able to:
- Define the term atrial fibrillation
- Be aware of the psychological impact of living with a long term condition such as atrial fibrillation
(including the screening tools available) - Understand the classification and causes of atrial fibrillation
- Recognise the signs and symptoms of atrial fibrillation
- Describe the treatment of atrial fibrillation to ensure an optimal quality of life
- Be aware of the stroke risk associated with atrial fibrillation and how that risk can be reduced
Introduction

Module authors
Module lead
Morven Dunn, Practice Development Nurse Practitioner-AF, NHS Lanarkshire / Practice Development Coordinator, BHF
Group members
Alison Keenan, Practice Nurse, NHS Ayrshire & Arran
Karen Smith, Consultant Cardiology Nurse, NHS Tayside, University of Dundee
Arlene Cobban, Atrial Fibrillation Nurse, NHS Fife
Mairi Chrystal, CHSS Head of Stroke Nurse & Specialist Services
Debbie Yorkston, Chief Physiologist, NHS Lothian
Sue Bryant, Cardiac Specialist Nurse, NHS Dumfries and Galloway
Anne MacDonald Practice Nurse NHS Greater Glasgow & Clyde
Steve McGlynn, Specialist Principal Pharmacist (Cardiology)
Jemima Traill, Senior Project Manager, BHF
Mairi Albiston, Clinical Psychologist, NHS Greater Glasgow & Clyde
Reviewers
Dr John Locke, GP, NHS Dumfries & Galloway
Dr Anna Choy, Consultant Cardiologist, NHS Tayside
Amanda Manson, Cardiac Specialist Nurse, NHS Orkney
Morag Osborne, Consultant Clinical Psychologist, NHS Greater Glasgow & Clyde
John Stout, GP, NHS Grampian
Neil Grubb, Consultant Cardiologist, NHS Lothian
Acknowledgement to Maureen Carroll, MCN Manager, NHS Lanarkshire (Atrial Fibrillation Audit and Education Project).
8. Atrial fibrillation
Learning outcomes
- Define the term atrial fibrillation.
- Be aware of the psychological impact of living with a long term condition such as atrial fibrillation (including the screening tools available).
- Understand the classification and causes of atrial fibrillation.
- Recognise the signs and symptoms of atrial fibrillation.
- Describe the treatment of atrial fibrillation to ensure an optimal quality of life.
- Be aware of the stroke risk associated with atrial fibrillation and how that risk can be reduced.
General Medical Disclaimer: The information, including but not limited to, text, graphics, images, recommendations, opinions and other material contained on or accessed through this website (or in any module or content accessible through this website) (together “Website”), is intended for general informational purposes only. The information should not be considered as professional medical advice, diagnosis, recommendations or treatment. The information on this Website is provided without any assurance, representations or warranties, express or implied. We do not warrant that the information on this Website is applicable to all healthcare practices, geographical locations, health needs or circumstances. We do not warrant that the information on this module is complete, true, accurate, up-to-date, or non-misleading. You should always seek the guidance of a qualified healthcare professional before making any decisions related to your health or wellbeing. Never disregard or delay seeking medical advice due to something you have read on this Website. The use of or any reliance placed on any information provided on or accessed through this Website is solely at your own risk. If you have any specific questions or concerns about your health, please consult a qualified healthcare provider or other qualified medical professional. Do not rely on the information on this Website as an alternative to medical advice from your doctor or other qualified professional healthcare professional or healthcare provider.
Module test

This is the module test for ‘HEARTe 7. Palliative care in heart disease’. It is strongly recommended that you work through the learning materials of the module prior to commencing this test. By going straight to the test you may miss out on valuable learning contained within the module. The answers to all the test questions are contained within the module. This information may have been provided in the ‘Additional Information’ boxes on some of the pages.
There are 10 questions and you must answer all of these correctly to obtain a certificate of completion.
You should allow approximately 10 minutes to complete the test.
Key messages
- Identify triggers that may suggest a declining change in the persons overall condition (frailty, co-morbidity, diminishing performance status etc).
- Review the evidence available to support the holistic assessment influencing the delivery of supportive palliative care for persons living and dying from advancing cardiac disease.
- Recognise the unique contribution of the MDT in optimising person-centred care.


