Bill’s preferred care wishes have been successfully facilitated at this time. Ongoing review and assessment of Bill’s needs and care wishes will be required to ensure or make certain that his care can be realistically sustained.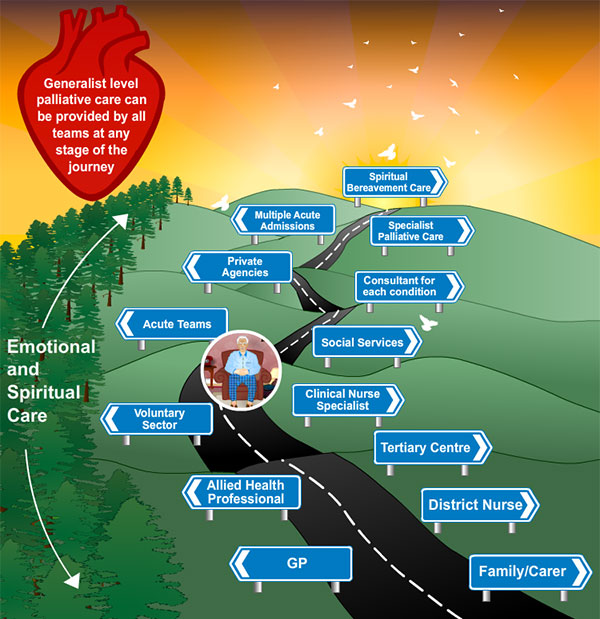
Category: HEARTe
The uncertain certainty
Heart failure/cancer disease trajectory (Murray et al 2005).
The rate of progression in individual patients is unpredictable. Three key factors contribute to the uncertainties experienced.
- Cardiac events which commonly precipitate hospitalisation, such as myocardial infarction, unstable angina, and AF can occur at any time
- Sudden death may occur at any point in the disease trajectory
- It can be difficult to identify when a patient is terminally ill
Reference: Scottish Partnership for Palliative Care
Specialist palliative care
General palliative care is appropriate for the majority of patients with advanced heart failure and should be incorporated into routine clinical care.
General palliative care includes provision of:
- information for patients and carers, with ‘signposting’ to relevant services
- accurate holistic assessment of patient needs
- co-ordination of care teams in and out of hours and across boundaries of care
- basic levels of symptom control
- psychological, social, spiritual and practical support
- open and sensitive communication with patients, carers and professional staff
- referral for specialist palliative care when necessary.
Referral for specialist palliative care
For people with complex needs specialist palliative care is provided by members of multi-professional palliative care teams, including consultants in palliative medicine, clinical nurse specialists, chaplains, social workers, pharmacists and appropriate allied health professionals. Specialist palliative care teams are available to advise colleagues in primary and secondary care as well as offering a specialist assessment or direct involvement in patient care if appropriate. In all care settings, an awareness of when to seek advice or refer can be crucial in ensuring that the palliative care needs of patients and families are met appropriately. Referral to specialist palliative care should not be regarded as ‘handing over’ the patient, but as an opportunity for the palliative care team to provide additional support to patients and carers and to their usual healthcare team as and when necessary at crucial points in the disease trajectory36. It has been estimated that no more than 10% of people with palliative care needs, including those with heart failure, are likely to require specialist palliative care.
Following referral to specialist palliative care the service may offer:
- a ward consultation by a palliative care doctor or clinical nurse specialist
- a visit for assessment or a short period of intervention by the specialist team in a hospital or community setting
- assessment in a specialist palliative care symptom control outpatient clinic
- assessment at a specialist palliative care day unit
- a short admission to an inpatient specialist palliative care or hospice unit.
Referral for a specialist palliative care assessment should be considered for the following:
- patients with difficult symptom control and / or complex physical or psychological family or social needs
- patients and families needing additional support with issues relating to end of life care including advance care planning and decisions about treatment and care.
Reference: Scottish Partnership for Palliative Care.
Financial considerations

Financial matters may be at the forefront of the thoughts of some palliative care patients, but it is often the last thing thought about. The following is not exhaustive but is a list of financial issues to be considered.
- For those patients who, unfortunately, are expected to have less than six months to live, they may automatically qualify for Personal Independence Payment and Employment and Support Allowance (if they are under 65), or Attendance Allowance (if they are over 65).
- The patient does not need to know a claim has been made – a DS1500 form can be supplied with most claim forms, with a box to indicate the person is claiming “Under Special Rules” or that a claim is being made on their behalf.
- The appropriate action is to suggest a referral to an appropriate service for Bill, and to make a referral with his consent.
- The financial support provided may enable Bill to address his decline in function and inability to see to ADL’s by directing his financial support as he wishes.
An example of an approach to reassessment of medication in advanced heart failure
A pharmacy review provides an opportunity to review and rationalise medication.
| Drug | Survival improved | Symptom control improved | Side effects* | Assessment/review |
|---|---|---|---|---|
| ACE inhibiter (angiotensin converting enzyme inhibitors) | yes | yes: less dyspnoea/fatigue; improves functional capacity; can reduce hospital admissions | cough, hypotension, lightheadedness, hyperkalaemia, renal impairment | Stop during any intercurrent illness which causes hypovolaemia. Caution if renal impairment or on other potassium conserving medication. Should ideally be reviewed by heart failure team. |
| Amiodarone | no | yes: by lessening dysrhythmias especially AF | hepatic dysfunction, photosensitivity, thyroid dysfunction, nausea. Important adverse interaction with other drugs which prolong the QT interval. |
Effective drug, but significant risk of adversely affecting quality of life. Very long duration of action. May take weeks-months for effect to be lost after discontinuation. |
| ARB (angiotensin receptor blockers) | yes | yes: as for ACE inhibitor | hypotension, lightheadedness, hyperkalaemia worsening renal function, | Stop during any intercurrent illness which causes hypovolaemia. Caution if renal impairment or on other potassium conserving medication. Should ideally be reviewed by heart failure team. |
| Aspirin | yes | no | GI irritation/haemorrhage | Stop if causing any symptoms. No proven role in non-ischaemic heart failure. |
| B Blocker | yes | yes: as for ACE inhibitor | fatigue/muscle weakness, nightmares, depression, cold peripheries | Stop or reduce dose if worsening dypsnoea or fatigue. Avoid abrupt withdrawal if possible. |
| Digoxin | no | yes: as for ACE inhibitor | nausea, vomiting, bradycardia/heart block, bigeminy | Risk of toxicity (e.g. in renal impairment) hence monitor levels. Risk of significant drug interactions. (see Appendix 1 BNF). |
| Diuretic | no | yes: breathlessness, oedema, can reduce hospital admissions | dehydration (uraemia), hypotension, hypokalaemia, gout (most effective agent in acute phase is low dose prednisolone; watch for fluid retention. Use allopurinol forlong term prevention once symptoms controlled) | Require regular monitoring and readjustment of dose. Likely to be needed until the last days of life. |
| Hydralazine | yes, with long acting nitrates | no | flushing, GI upset, hypotension, systemic lupus syndrome with long term use | Very limited role. Only used if ACE inhibitor and ARB intolerant. |
| Nitrates | yes, with hydralazine | yes: sublingual nitrates may lessen dyspnoea | headaches | Standard treatment for angina. Very limited role in advanced heart failure. Only used if ACE inhibitor and ARB intolerant. |
| Spironolactone | yes | no | hyperkalaemia, GI disturbance, breast tenderness, gynaecomastia with spironolactone | Stop during any intercurrent illness which causes hypovolaemia. Stop if potassium rises (>5.5mmol/L). |
| Statin | yes | no | nausea, hepatic dysfunction, myalgia | Stop if side effects, and do not replace with other drugs. |
| * see current version of BNF or Summary of Product Characteristics for full list.
Note: advice on these issues can be sought from the most appropriate member of Bills care team which may be the GP, palliative care team or heart failure nurse |
||||
Reference: Scottish Partnership for Palliative Care (2008) Living & Dying with Advanced heart failure: a palliative care approach.
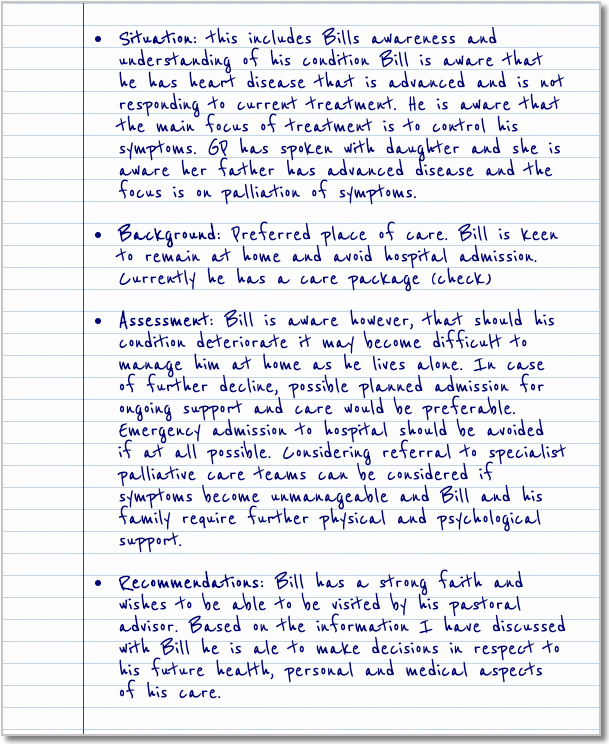
Bill’s immediate and anticipated care wishes
3 weeks later the nurse visits Bill to assess his condition. HF symptoms stable, daughter visiting and care package continues.
Bill’s Advanced Care Planning (ACP)
ACP is a voluntary process of discussion about future care between an individual and their care providers, irrespective of discipline. If the individual wishes, their family and friends may be included. It is recommended that with the individual’s agreement this discussion is documented, regularly reviewed, and communicated to key persons involved in their care.
An ACP discussion might include:
- The individuals concerns and wishes.
- Their important values or personal goals for care.
- Their understanding about their illness and prognosis.
- Their preferences and wishes for types of care or treatment that may be beneficial in the future and the availability of these.
The Anticipatory Care Plan can come in all different formats for different areas and should be individualised.
Bill’s care wishes
Implementing Bill’s care wishes requires effective verbal and written communication which should be shared with all members of the multi-disciplinary team. The professional who knows Bill well and who has a good relationship with is best placed to co-ordinate the sharing of information.
Aligning preferred care wishes with actual place of care and death
Professionals who could be involved with Bill’s care
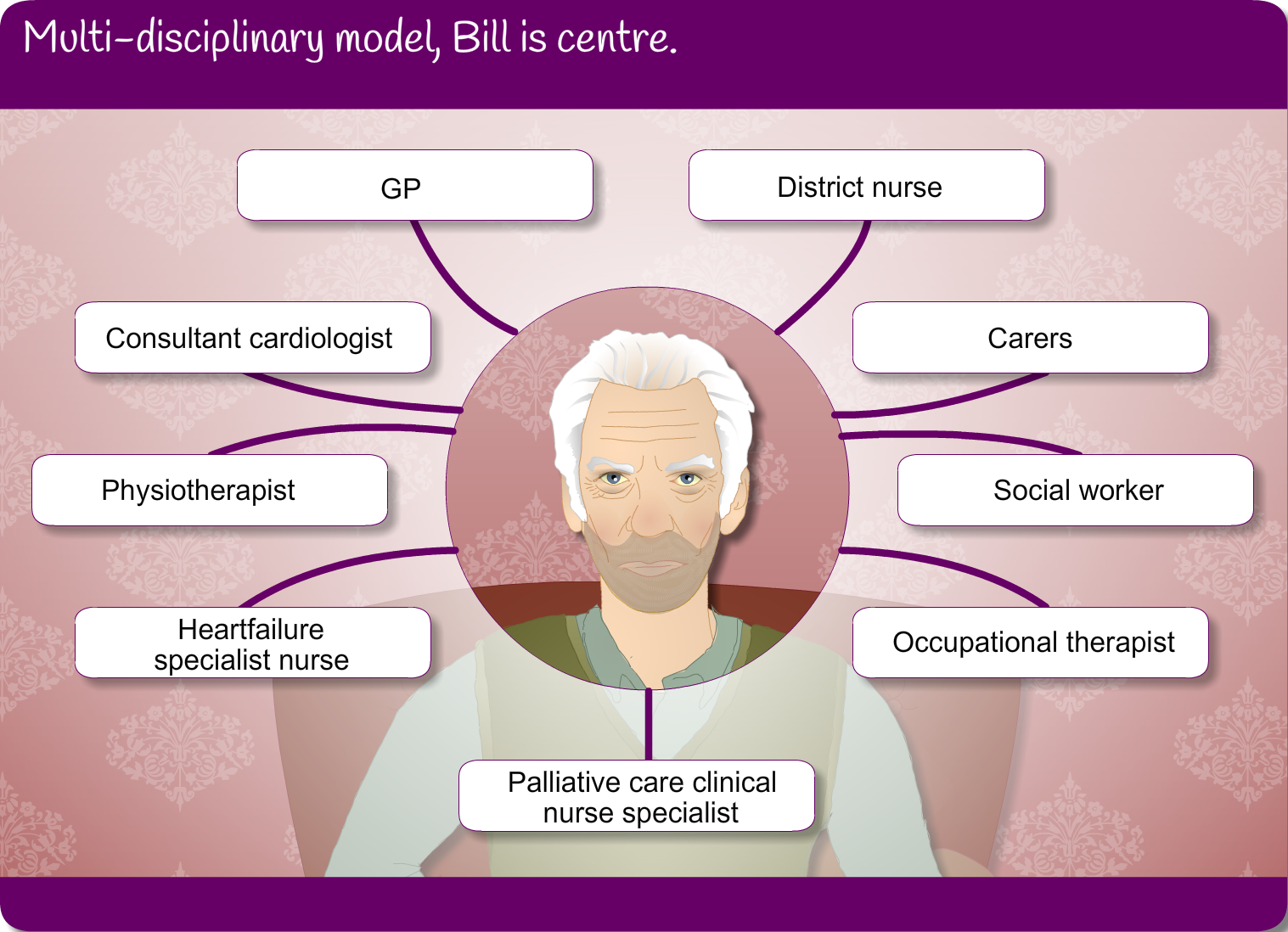
Collaborative working with a wide range of professionals may be required to optimise Bills ongoing care. Professional input will vary across different geographical areas and will be responsive to patients needs.


