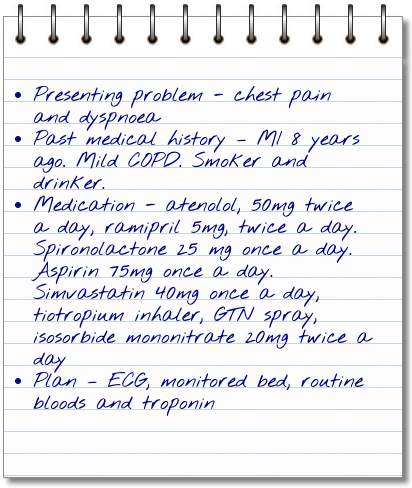
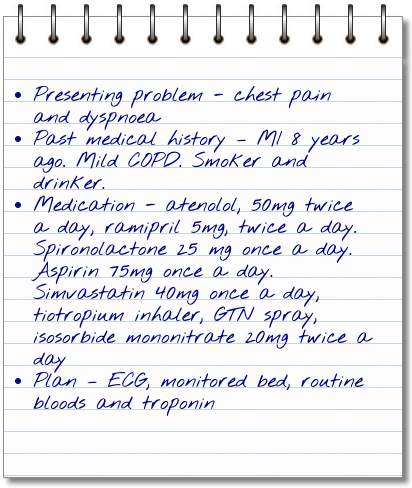
Frank’s notes suggest he may have acute HF, lets examine some other causes of acute HF.
| Common causes of acute HF |
| Cause |
Precipitating factor |
Rationale |
| Ischaemic heart disease (also known as coronary artery or coronary heart disease) |
- Acute Coronary Syndromes (see Module 4)
- Myocardial infarction
- Right ventricular infarction
|
When the cardiac muscle is damaged or has any insult, it can become less competent in its pumping action, leading to acute HF |
| Valvular |
- Valve stenosis
- Valvular regurgitation
- Endocarditis
- Aortic dissection
|
When the valves do not work effectively and allow blood to move unchecked within the heart the pumping action can become affected |
| Circulatory failure |
- Septicaemia
- Thyrotoxicosis
- Anaemia
- Shunts
- Tamponade
- Pulmonary embolism
|
When the body’s other systems endure insult or injury, the heart must work harder to compensate and if overwhelmed or prolonged this can lead to acute HF |
| Arrythmias |
- Atrial fibrillation
- Ventricular arrhythmias
- Tachycardias
- Bradycardias
|
If the rhythm of the heart is disturbed for any reason, the pumping action of the heart becomes less uniform and can lead to acute heart failure |
| Decompensation of pre-existing chronic heart failure |
- Lack of adherence
- Volume overload
- Infections, especially pneumonia
- Cerebrovascular insult
- Surgery
- Renal dysfunction
- Hypertension/arrhythmia
- Respiratory disease
- Hypertension
- Drug abuse
- Acute Arrhythmia
- Alcohol abuse
|
Early recognition of signs and symptoms of heart failure as discussed within self management can reduce the risk of acute heart failure. However some of these precipitating factors can be due to additional co morbidities or lifestyle issues.
Non compliance with medications (specifically diuretics) is a common cause of increasing symptoms including fluid retention. Establishing a rapport with patients and discussing this aspect specifically is important in increasing concordance. |
Reference: ESC Acute and Chronic Heart Failure Guidelines
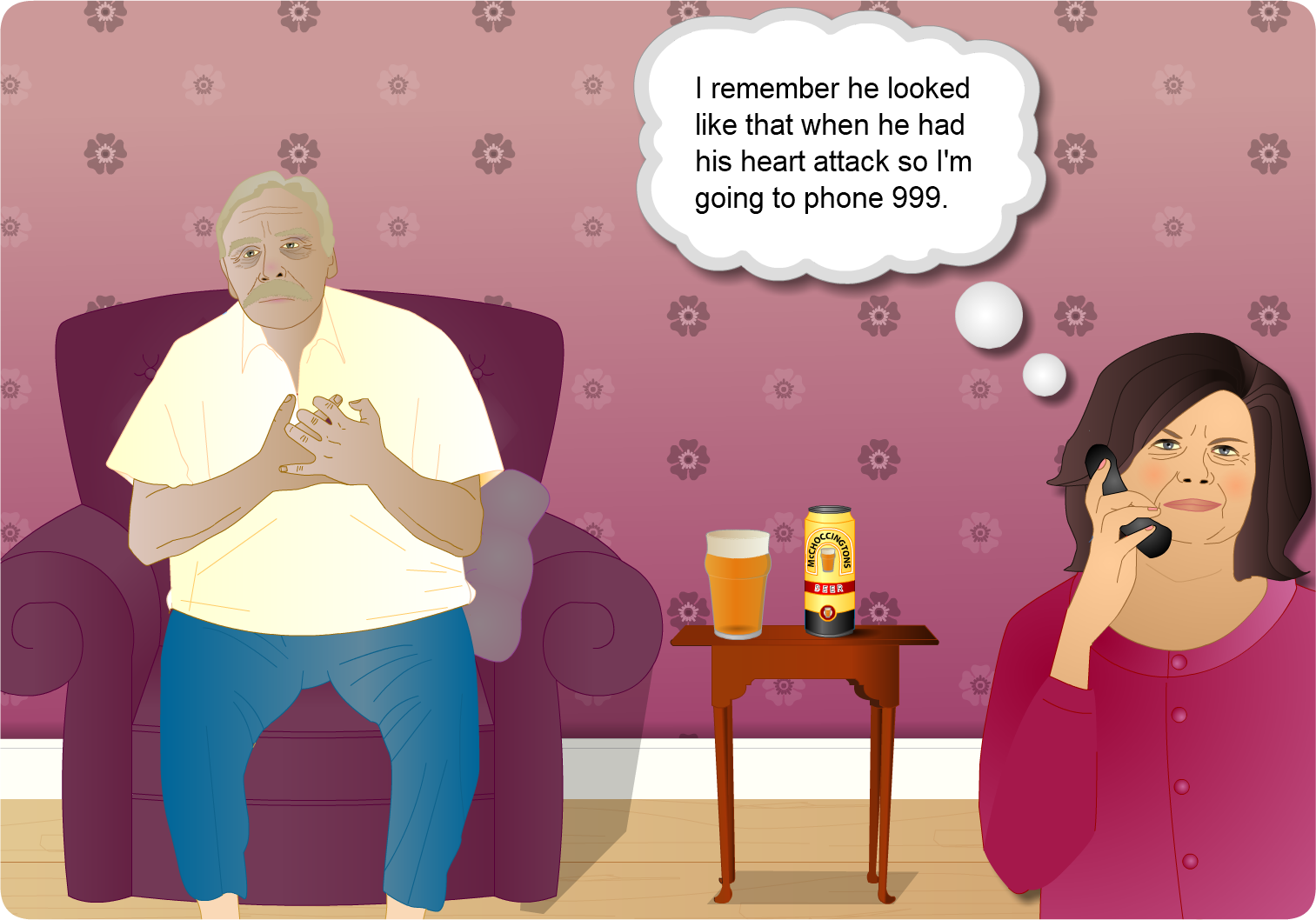
Frank is unable to lie flat and is he is struggling for breath: Frank may be unable to lie flat due to fluid building up within his body tissues and then being redistributed to his lungs when he lies down due to fluid body position. This means his lung tissues become “water logged”.

This is the module test for ‘HEARTe 6. Heart Failure’. It is strongly recommended that you work through the learning materials of the module prior to commencing this test. By going straight to the test you may miss out on valuable learning contained within the module. The answers to all the test questions are contained within the module. This information may have been provided in the ‘Additional Information’ boxes on some of the pages.
There are 10 questions and you must answer all of these correctly to obtain a certificate of completion.
You should allow approximately 10 minutes to complete the test.

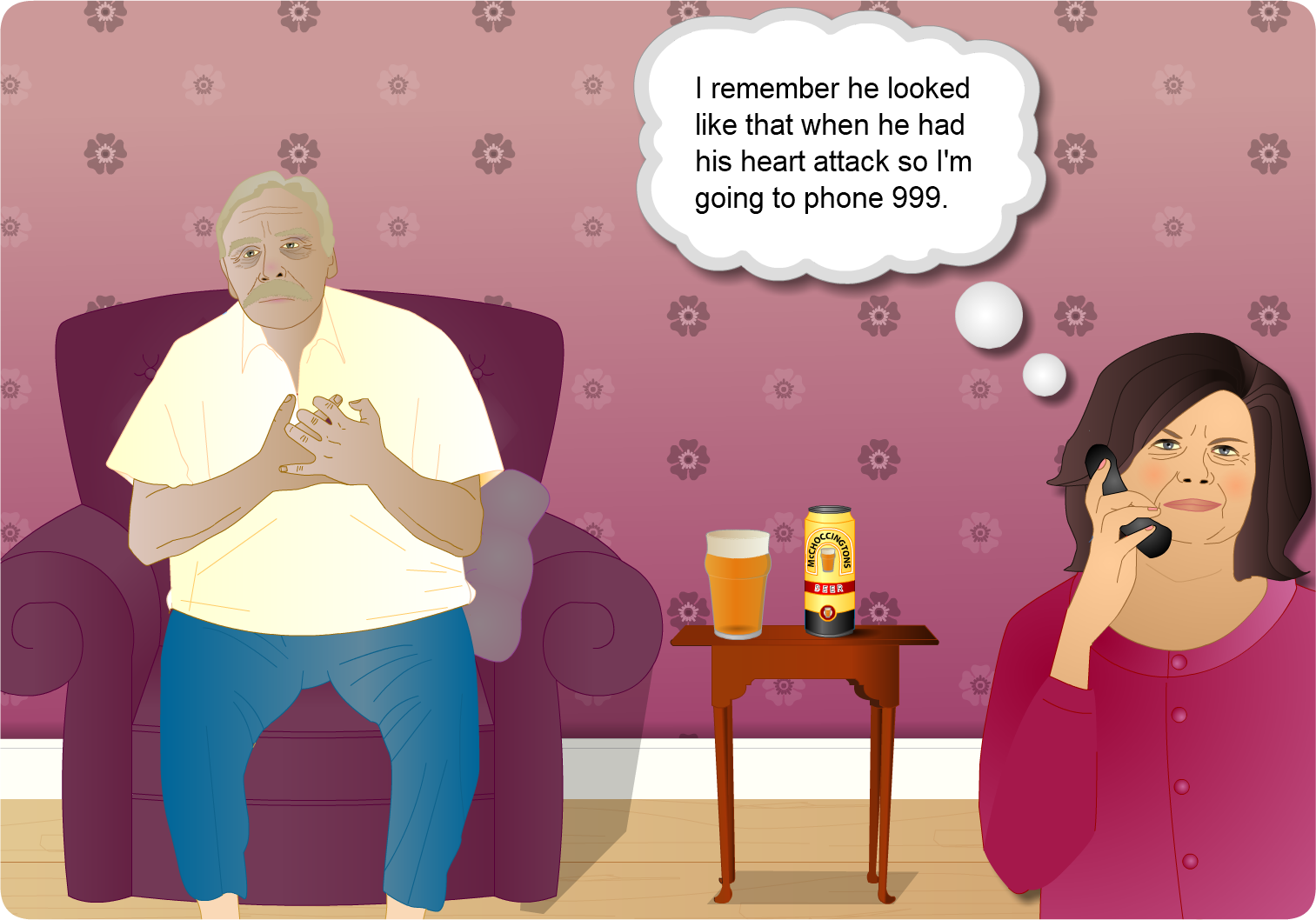
Frank is a 60 year old man who works as a bus driver. He has had a previous myocardial infarction 8 years ago. Frank is a smoker and drinks alcohol regularly. He lives with his wife Betty. He enjoys socialising and is a member of his local darts team. Recently he has felt more tired and slightly more breathless.
By the end of this case you should:
- Be aware of the trajectory in HF and the care and support patients require
- Develop an awareness of the non-pharmacological and pharmacological management of HF
- Identify HF symptoms and be aware of the NHYA tool and the assessment of patient’s symptoms.

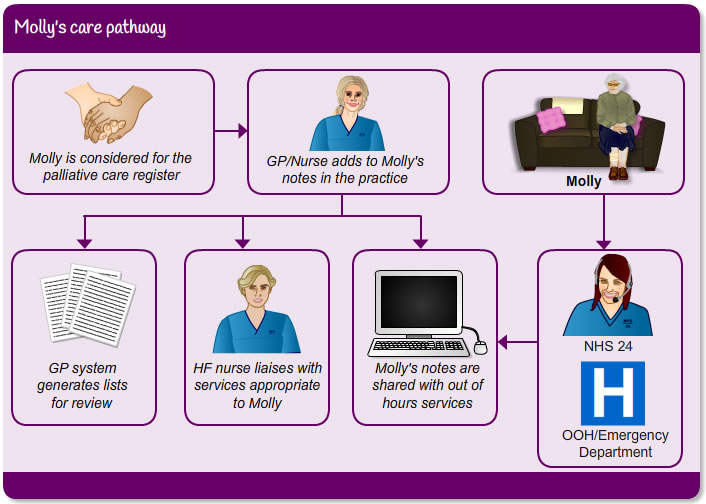
The trajectory of Heart Failure (HF) is often unpredictable but for someone with Molly’s co-morbidities and HF progression, a supportive and palliative approach to her care is appropriate. Molly is now being followed up by the heart failure nurse service and the palliative care team will be involved if and when appropriate. Learn more about the supportive and palliative care approach in Module 7.
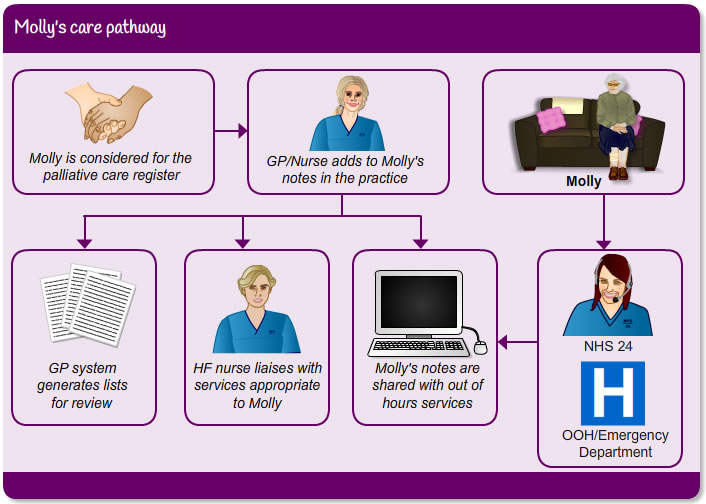
ePCS/eKIS:
ePCS/eKIS is a significant development which allows GPs and District Nurses to record information on the palliative and end of life needs of their patients onto their GP software system, and for this to be available to those providing care in the Out of Hours period. For more information see Module 7 or access the Scottish Government website.
DNACPR:
Clinicians working across NHS Scotland are able to make decisions regarding the appropriateness of Cardiopulmonary Resuscitation (CPR), issuing a DNACPR instruction if considered clinically appropriate.
The responsibility for deciding if resuscitation is in the patient’s best interests lies with the patient’s lead clinician and any decision made regarding CPR will be based on a full consideration of the patient’s case.
Scottish Government have introduced a policy intended to prevent inappropriate, futile and/or unwanted attempts at CPR which may cause significant distress to patients and families as a death with an inappropriate CPR attempt may be undignified and traumatic. When a patient dies at home or in a care home an inappropriate CPR attempt is likely also to involve the Scottish Ambulance Service paramedics and even the police, which can add greatly to the distress for the families and be upsetting for all those involved. This policy is intended as a positive step to help a person’s wishes to be followed at the end of life irrespective of whether they are being cared for in hospital, hospice, care home or in their own homes. There is much confusion and uncertainty about CPR and the process of making advance decisions that CPR should not be attempted. Variations in local policies can cause misunderstandings and lead to distressing incidents for patients, families and staff. Increased movement of patients and staff between different care settings in Scotland makes a single integrated and consistent approach to this complex and crucial area a necessity. Access for further info:
NHS Scotland: Do Not Attempt Cardiopulmonary Resuscitation [PDF]
Adequate communication is vital when considering integrated palliative care approach to care for Molly´s wishes. Alongside these, DNACPR should be considered so the person´s competency can be assessed to make make the best decisions for the future.

The HF nurse tells the GP she has been out to see Molly and that she doesn’t seem to be progressing well overall. She tells her that Molly has expressed a desire to stay at home however unwell she becomes. They agree that further discussions need to happen to plan the most appropriate way forward, with Molly’s wishes central to this process.