 The heart failure nurse checks that she understands what Molly has told her about her current condition. Molly’s symptoms have improved and she is now less oedematous but her breathlessness is still problematic. The HF nurse reminds Molly that previously the cardiologist had decided that surgery was not an option for Molly and that her symptoms should be managed by medication. She tells her that discussions should perhaps take place between Molly and the multi disciplinary team regarding her future care. The nurse then discusses aspects of this care in more detail, including discussing with Molly her thoughts about her preferred place of care. Molly tells the HF nurse she really wants to stay in her own house if she can.
The heart failure nurse checks that she understands what Molly has told her about her current condition. Molly’s symptoms have improved and she is now less oedematous but her breathlessness is still problematic. The HF nurse reminds Molly that previously the cardiologist had decided that surgery was not an option for Molly and that her symptoms should be managed by medication. She tells her that discussions should perhaps take place between Molly and the multi disciplinary team regarding her future care. The nurse then discusses aspects of this care in more detail, including discussing with Molly her thoughts about her preferred place of care. Molly tells the HF nurse she really wants to stay in her own house if she can.
Category: HEARTe
Emotional assessment
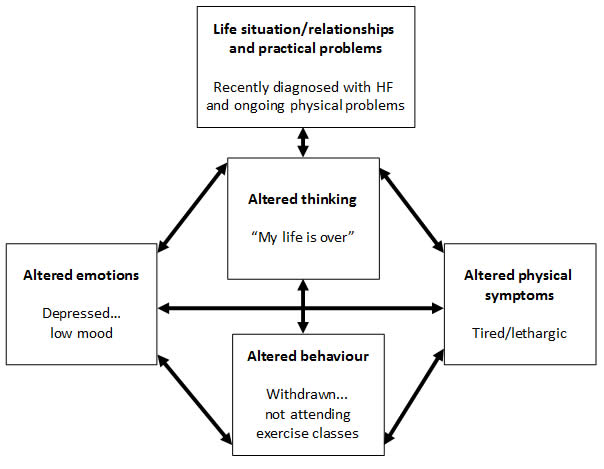
From the diary it obvious that Molly is looking at life from a negative aspect. This prompts the nurse to look in depth at her emotional feelings.
One of the following tools used is the pHQ-9, click here for more information.
Consider asking the following 2 questions to start an assessment of depression
- During the last month, have you often been bothered by feeling down, depressed or hopeless?
- During the last month have you often been bothered by having little interest or pleasure in doing things?
If Molly answers yes to EITHER identification questions, ask the following 3 questions
- During the last month have you often been bothered by feelings of worthlessness?
- During the last month have you often been bothered by poor concentration?
- During the last month have you often been bothered by thoughts of death?
Consider using a validated measure for further evaluation, PHQ-9
If Molly is assessed to be at risk of suicide or deliberate self-harm:
- take into account toxicity in overdose if an antidepressant is prescribed or if necessary, limit the amount of drug(s) available
- consider increasing the level of support, such as more frequent direct or telephone contacts
- consider referral to specialist mental health services
HF nurse assessment
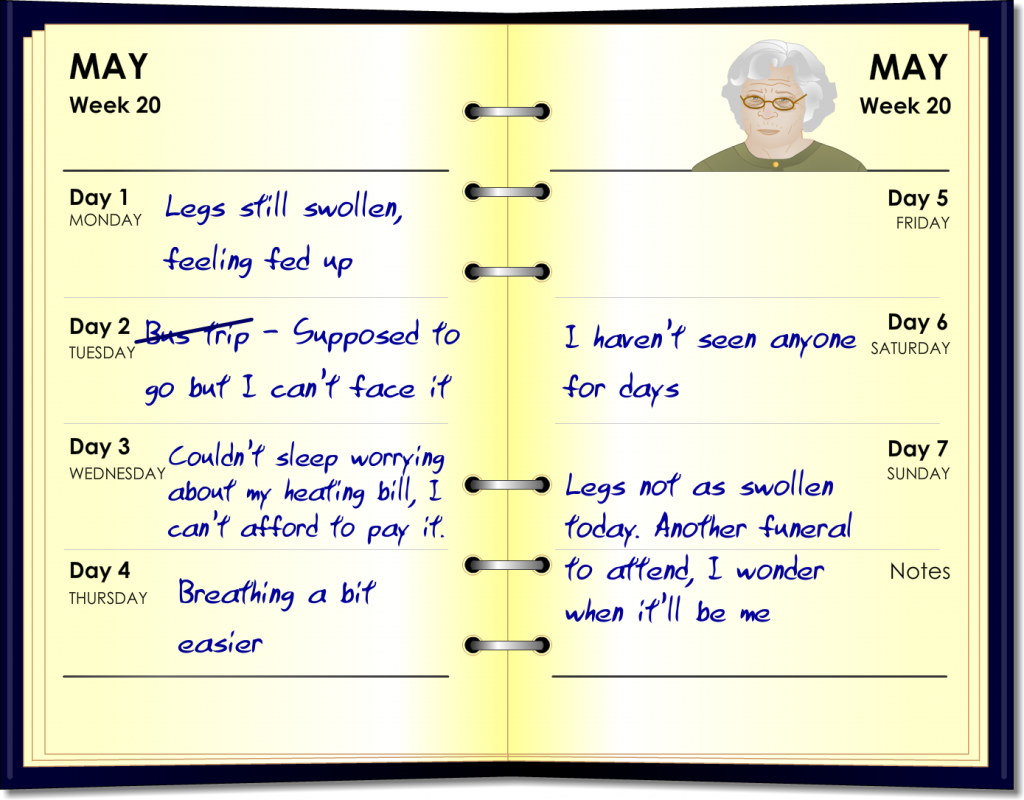
Although a physical assessment will be undertaken at each visit (see assessment sheet), it’s important for the nurse to consider Molly’s emotions as well as her physical symptoms. Looking at Molly’s diary, although her symptoms are beginning to improve (legs are less swollen today) her mood is low as she is cancelling day trips out and talking about her friends dying and wondering when it will be her.
Below is an example of a specialist HF nurse assessment using a structured approach. HF services across Scotland may use a slightly different tool, but the information is the same.
The HF nurse visits Molly
The HF nurse visits Molly after receiving a referral from the GP. She asks if Molly has been able to keep the diary that the practice nurse had suggested. Molly shows her the diary.
Molly’s self management plan
The key to successful management of long term conditions ultimately rests in the hands of the person who lives with the condition and their ability and aspiration to care about themselves, however they may require support to self manage. (COSMIC 2013)
Anticipatory care tries to consider these factors in supporting self management.
- Self Care: What each person does on an everyday basis. This is often compromised for a person living with a long term condition such as heart failure.
- Self Management: The process each person develops to manage their condition.
The practice nurse talks with Molly
Rationalisation of medication
The practice nurse discusses Molly’s medication with her before she goes. It is important to check that Molly is taking all these tablets and also any over the counter medications that she may be taking.
Ask your patient at each visit “has anyone changed, stopped or started any tablets for you since I saw you last?”. This simple question will remind them to inform you of any changes. Rationalisation of medications is an important part of Molly´s management plan which is to up-titrate evidence based therapies such as ACE inhibitor and Betablocker, while stopping or changing those which are of no benefit or indeed contra-indicated in heart failure.
The next day
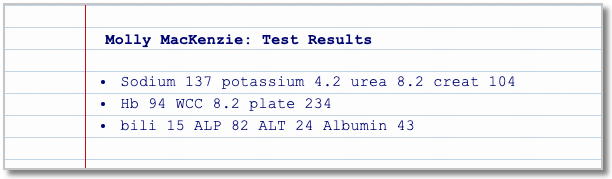
Molly’s blood tests are back and the GP discusses the results with the practice nurse. The GP tells the practice nurse he is making a referral to the specialist Heart Failure (HF) nurse service.
Molly’s immediate management plan

The GP tells Molly that there are more things she wants to discuss but needs to ensure she gets home safely today. Molly is happy to go home so the GP books her a taxi and books her an appointment for the next day.
| Findings | Linked to Molly’s heart failure | Outcomes |
|---|---|---|
| Review medications | May be worsening Molly’s HF e.g. pioglitazone and any non steroidal anti-inflammatories (NSAID) | Timely review of medications and alternatives as may affect other co-morbidities |
| BP 90/60(sitting) 80/50 (standing) |
Dizziness is worse when standing | Split timing of diuretic and beta-blocker. Advised to rise slowly to improve dizziness |
| Pulse 66 and regular | Molly is on multiple medications which can affect pulse rate and rhythm | Rationalise medications – see next screen |
| NYHA class III – (see Additional Information) | NYHA class is deteriorating as she has increased breathlessness and oedema | Diuretic compliance. Incontinence issues explored |
| Routine blood tests | Molly’s symptoms could be linked to worsening blood results | Await results in meantime discuss fluid and dietary intake |


