Many structured cardiac rehabilitation programmes encompass both an exercise and education programme. Programme lengths, frequency and format vary. Irrespective of format, the exercise component must include a warm up, conditioning phase and cool-down. Exercise prescription can be adjusted to meet the requirements of the patient. For health benefits, patients are encouraged to adopt an active lifestyle and incorporate physical activity into their daily routine. The recommendations to achieve this are to accumulate 30 minutes of moderate intensity physical activity on most days of the week. If the patient goal is to improve cardiovascular fitness then 2 -3 sessions of 45-60 minutes of continuous moderate intensity activity is recommended (inclusive of a 15 minute warm up and 10 minute cool down). Exercise should be monitored using heart rate, blood pressure, rating of perceived exertion (RPE), observations, or a combination of these.
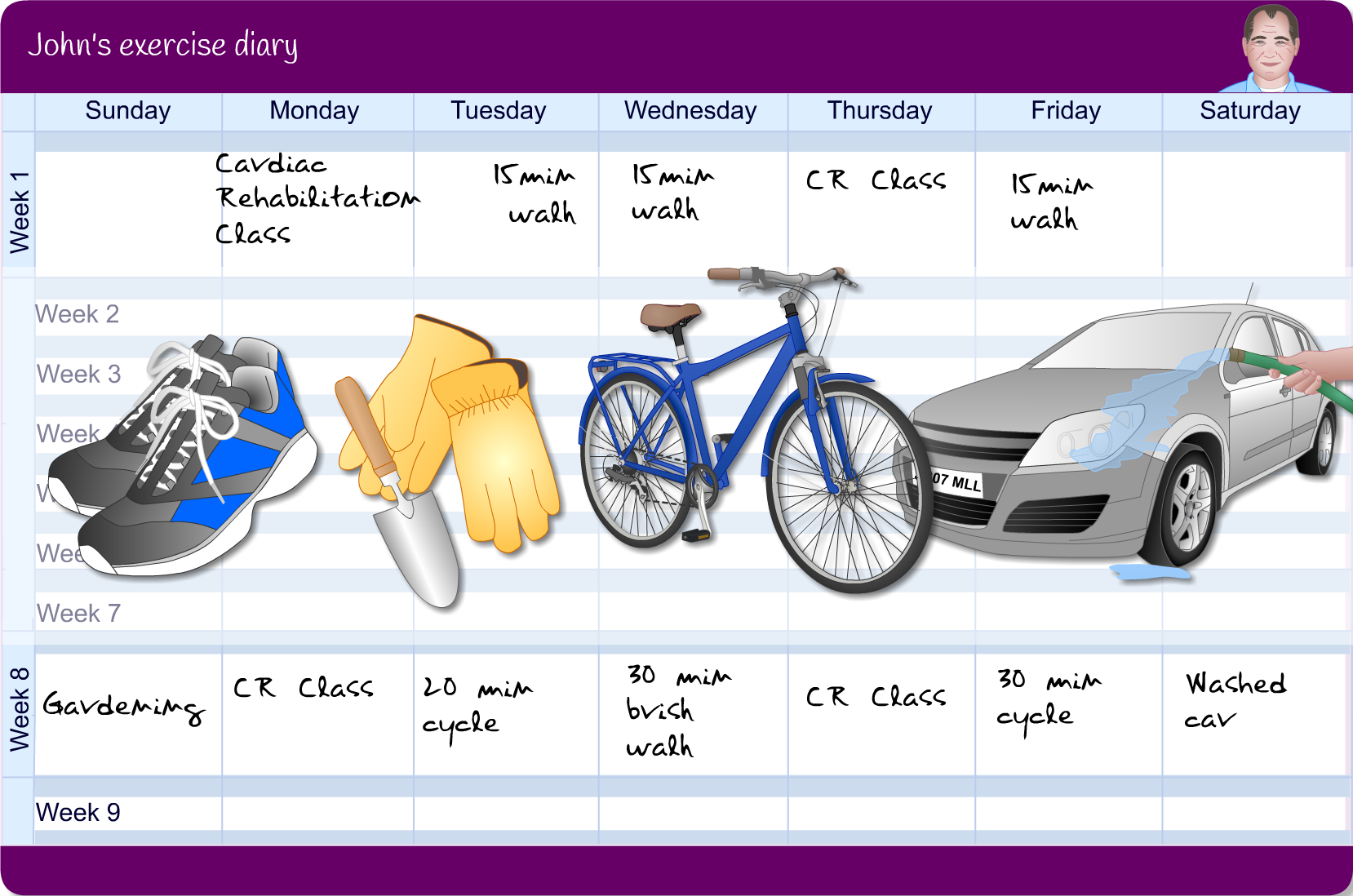
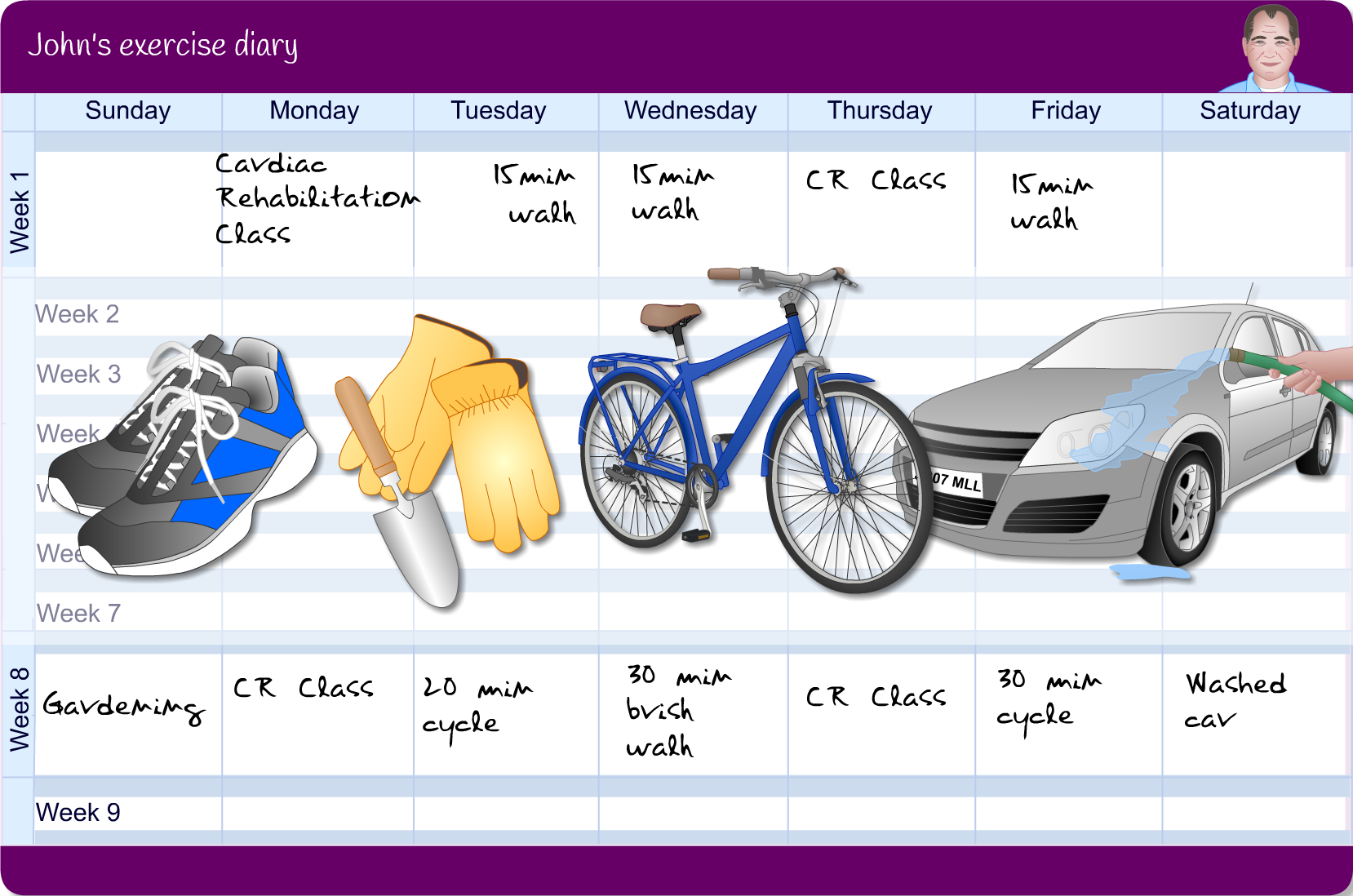
A rehabilitation goal should be the self-monitoring of all physical activity and exercise by the patient. Consider Johns diary and how his activity has begun to form part of his changing lifestyle.
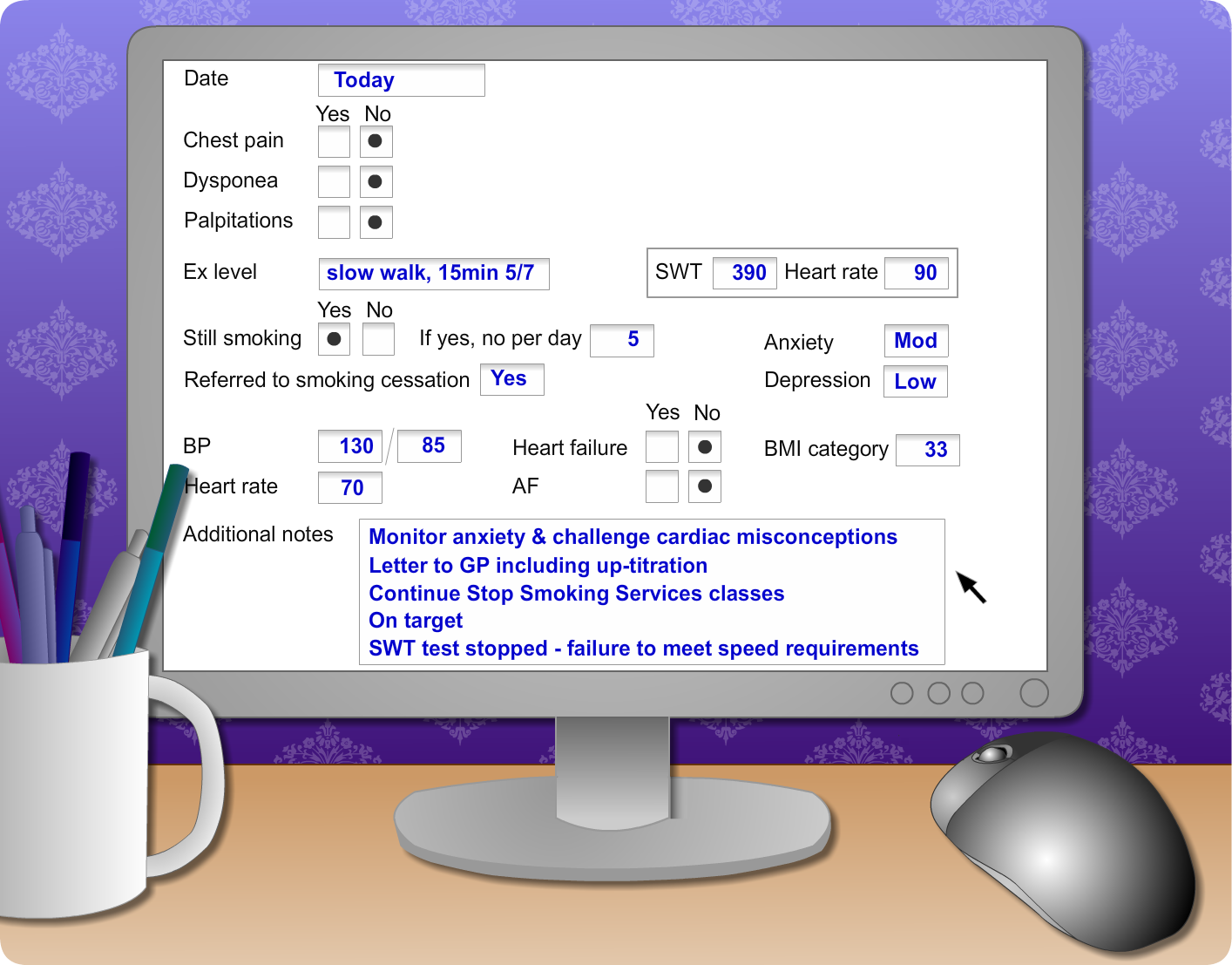
John was not found to be severely anxious- but if he was he would have been referred to psychology service, which vary from area to area in accessibility and service provision. The importance of early identification of clinical depression and anxiety is recognised within cardiac rehabilitation and there should be a protocol in place for local referral to specialist psychology services.
Stress Management is part of the integrated approach to CR programmes and will vary but generally contain the following as part of the whole education programme.
- causes and symptoms of stress
- types of relaxation including compassionate mindfulness
- goal setting
- challenging negative thinking
- assertiveness
- sleep clinic
- problem solving
This can increase patients confidence and all aspects of their recovery can improve including activities.
Being able to identify and reframe misconceptions is a skilled task and is informed by the principles of Health Behaviour Change (HBC). It is important to build rapport and to not dismiss misconceptions outright. Rather, explore where the misconception has come from and ask permission to give some further information, then elicit their thoughts about it. This can be done with patient and family or together. It is important to listen to these common misconceptions as if they are not addressed and recognised, can lead patients to demonstrate anxiety.
John attends his out-patient cardiac rehabilitation follow up. Look over Johns results on the screen to see the changes he has made in the goals he set during the agenda setting session.
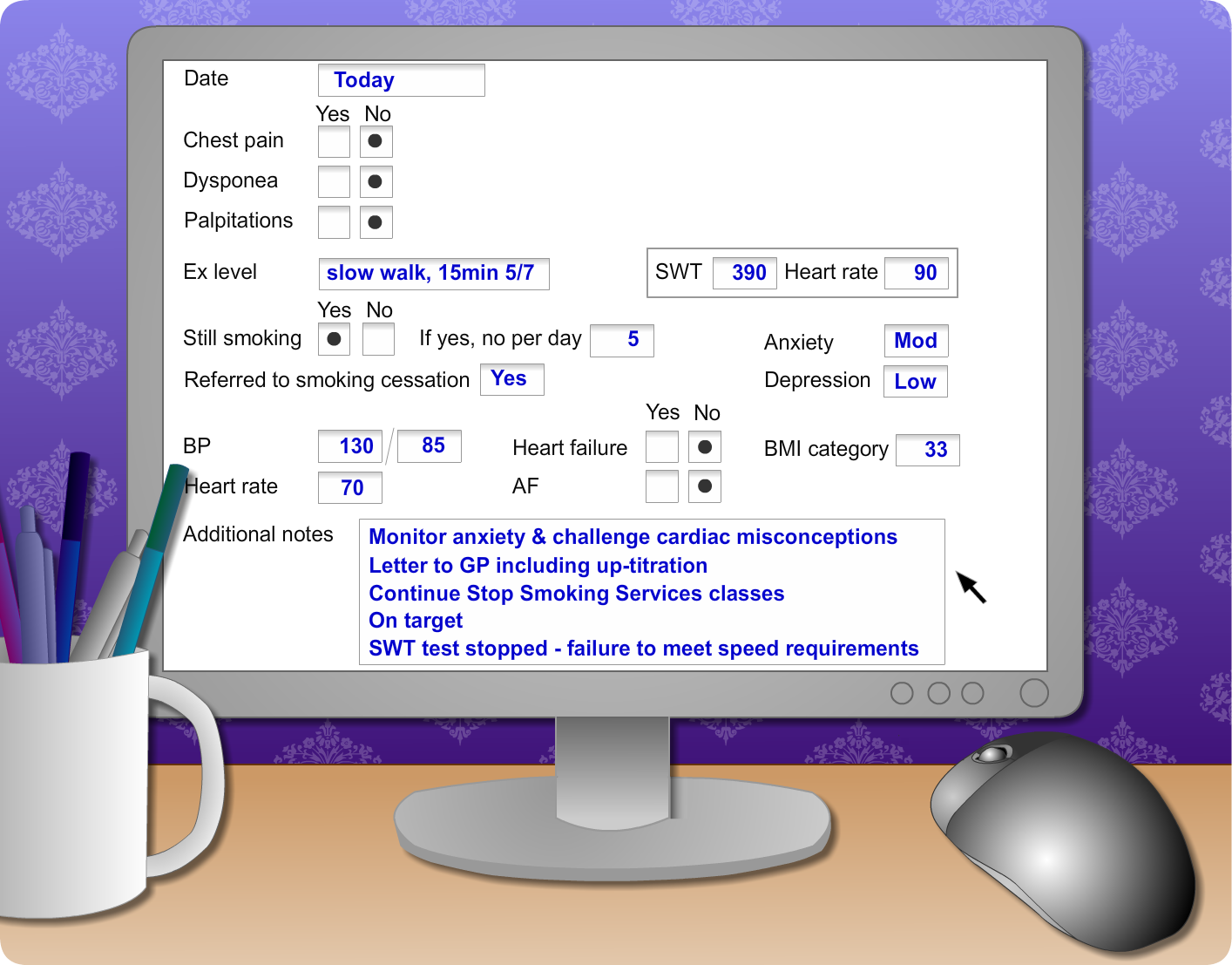
John’s anxiety and depression scores will have been achieved when he is assessed using a validated mental health screening tool. He was not found to be severely anxious but if he was he would have been referred to a psychology service. Referral and access will vary from area to area.
Lets look at the medications we would expect for Johns post-discharge prescription as he requires life long secondary prevention of cardiac events.
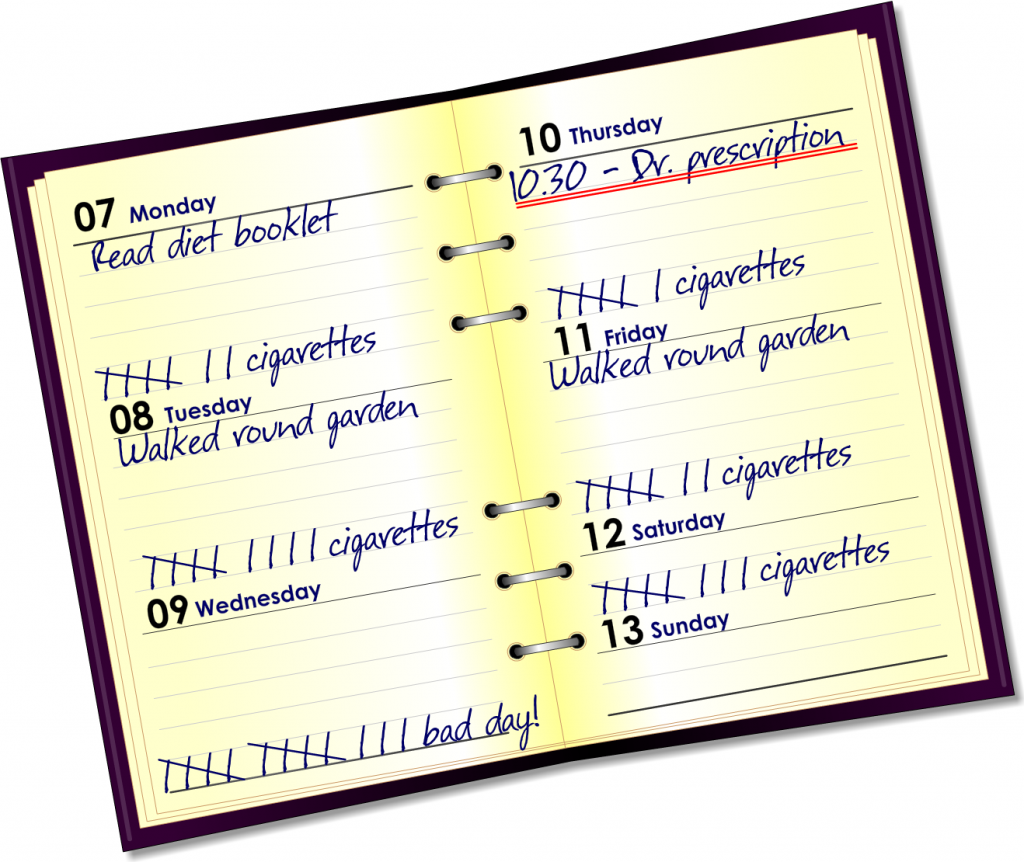
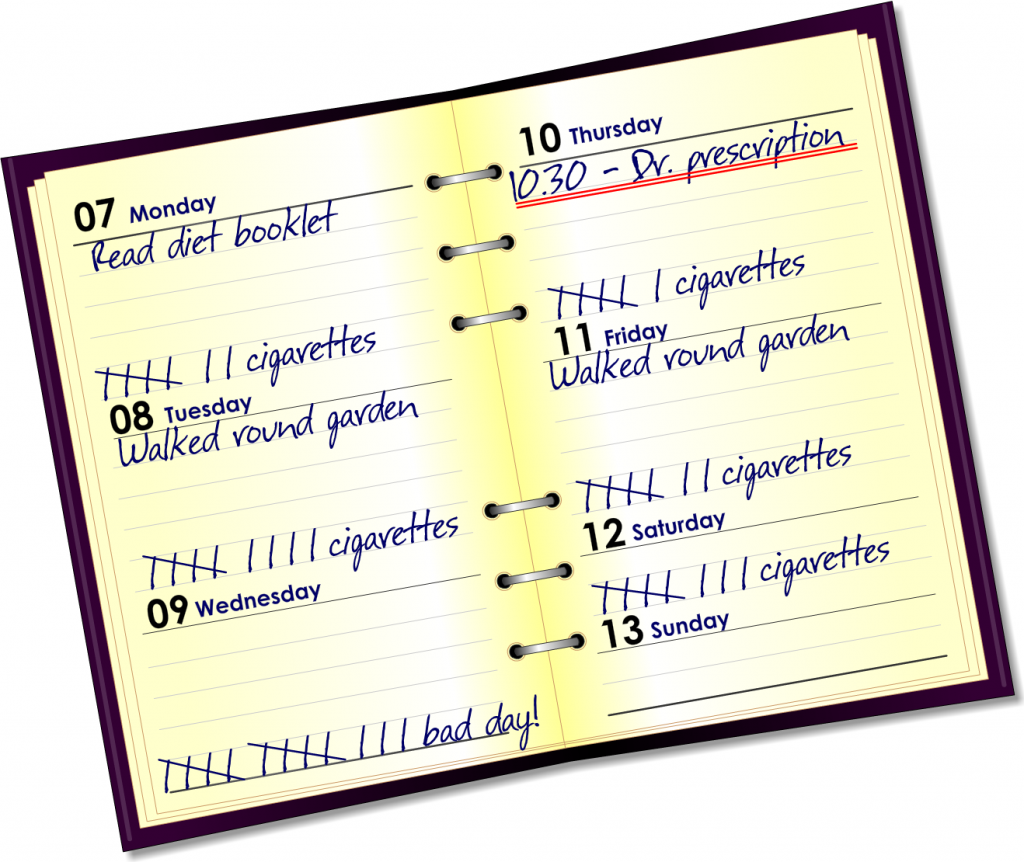
As you can see from John’s diary it can be really useful in recognising changes in emotional and physical well-being and can be used as part of a holistic assessment as well as gauging activity and lifestyle issues. John is trying to cut down his cigarettes and is documenting his activities.
He has accessed his prescription and has not written that he is experiencing any adverse effects or symptoms since discharge.
John is discharged from hospital after 4 days and goes home after an uncomplicated stay. He has a letter to hand into his GP and a prescription for his medication which was explained by the ward pharmacist.
John leaves with verbal and written information and an appointment to see the CR dietitian. He is given information on activities he can do and has been asked to keep a diary of his first week at home to discuss with the CR professional when he sees her within 10 days. This is something that the CR professional explains will be useful for him to review in a few weeks time to provide affirmation of his recovery.
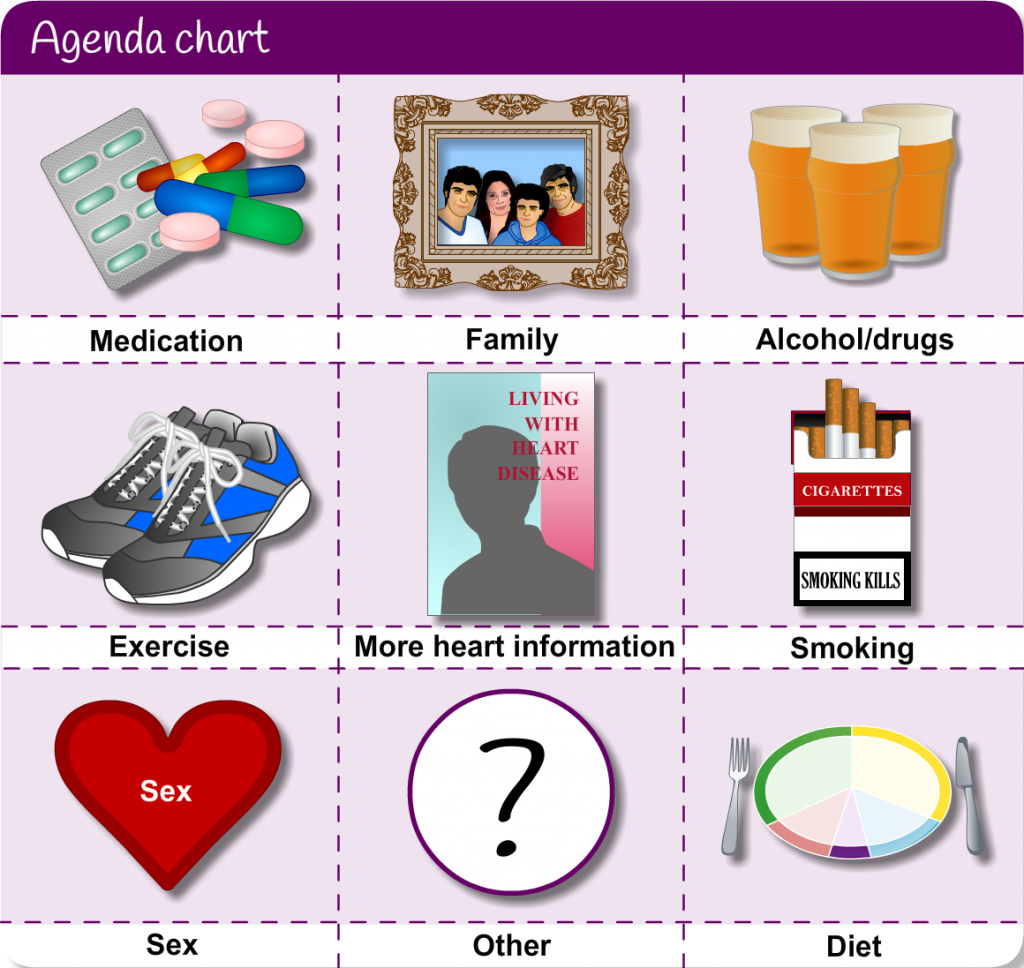
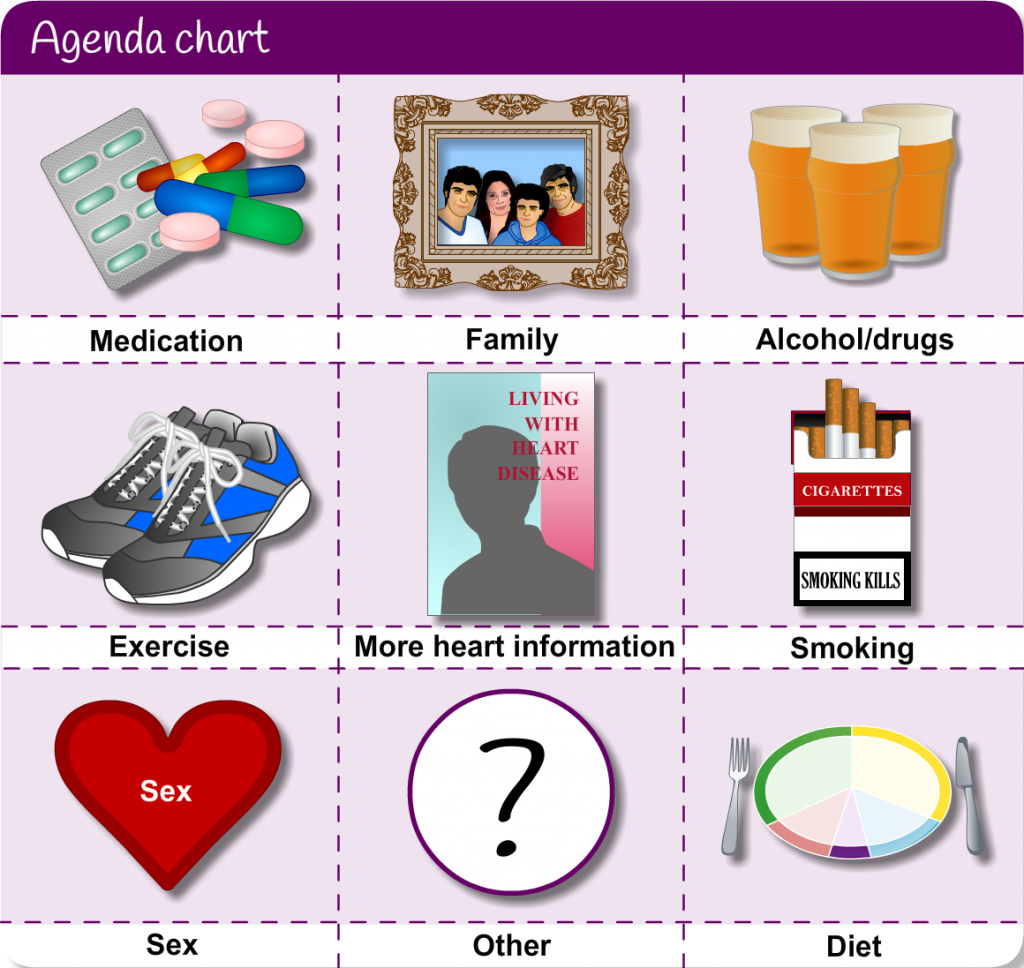
John considers these in relation to his diagnosis of heart disease and identifies smoking and his diet as two areas he thinks he could look at changing.
The cardiac rehabilitation (CR) professional discusses the readiness ruler and discusses referring him to stop smoking services. (learn more about the options within stop smoking services within module 2). Smoking is one of the major risk factors of CHD and substantially increases the risk of having a further heart attack. People who succeed in stopping smoking reduce the chances of having another MI by 50% in the first year. She explains that there are well known toxins in just one cigarette including tar (causes lung cancer, carbon monoxide (is a poisonous gas) and nicotine (which is addictive and narrows heart arteries (coronary arteries).
Poor diet is another modifiable risk factor that John could address with a look at healthy alternatives and the introduction of different food types. She tells John she will refer him to the CR dietitian for further input when he gets home but directs him to the booklets and web resources he could look at meantime.
She tells John that from his dietary recall, he has a high intake of high energy snacks, and fried foods with low intakes of fruit and vegetables which is contributing to weight gain.
John continues his CR assessment in the day area of the ward the next day. This assessment will integrate both physical and psychological components using behavioural change approaches.
Agenda setting is a good way to focus on the main concerns and avoid lecturing the patient or ‘talking in monologue’ is to use the agenda setting technique. Let’s look at these in relation to John.
The CR nurse encourages John by using an agenda setting tool which illustrates areas of lifestyle management that she asks John to consider.
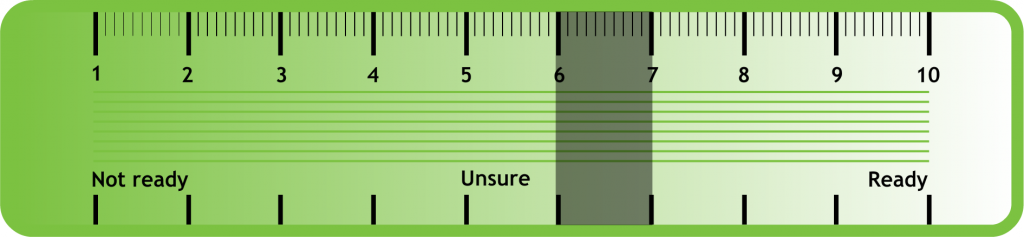
Carol the CR nurse then asks John to consider how important these changes are to him and how confident he is to change using another tool called a Readiness Ruler.
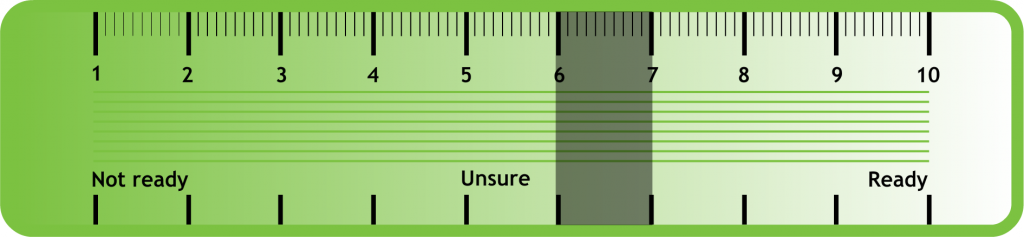
The Readiness Ruler – Is a structured and directive way of enabling patients to say how they feel about a particular change within a couple of minutes.
The cardiac rehabilitation professional visits John and explains what has happened to him. John has had a ST-segment-elevation myocardial infarction (STEMI), another name this is given is a heart attack. It is important to consider patient friendly words to ensure they understand what has happened to them and explain the process that occurred to address any cardiac misconceptions.