The upper arm is used to measure BP because it reflects the central aortic pressure. It is good practice to check BP in both arms, to identify any significant variation in measurements. Inside the cuff is the bladder, which requires to be the correct size to measure the BP correctly.
Category: HEARTe
Measuring BP in practice – 1
Further resources
The following link has a range of useful further reading and resources including educational videos.
Blood Pressure (BP)
BP is the force or pressure that blood exerts upon the vessel walls. The pulsatile ejection of blood from the left ventricle allows blood to flow from a high pressure area to lower pressure parts of the body. Blood pressure reflects the arterial pressure in the systemic circulation. It varies with each heart beat between a maximum value during systole and a minimal value in diastole. The difference between Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) is called the pulse pressure. The most significant pressure is the Mean Arterial Pressure (MAP). MAP is calculated using the following equation: MAP=DBP (SBP-DBP divided by 3). This is shown on most automated BP machines and reflects the pressure at which blood flows through the body and at which organs are perfused.
British & Irish Hypertension Society: With Automatic Blood Pressure Monitors [PDF]
British & Irish Hypertension Society: With Manual Blood Pressure Monitors [PDF]
There are a variety of monitors available for clinical use. What type do you use? Best guidance is available from these links below. All kite mark monitors undergo a testing process when they first are on the market and they are graded by a UK or European protocol rating, as the links describe. Make sure any new monitors you get are fit for purpose by following these links. Older monitors are usually the earlier types of those mentioned in the links, and should be satisfactory if they are similar to the ones listed in the links.
Pulse
Taking a manual pulse is essential when reviewing a patient. Not relying on electronic monitor readings of a pulse means that the practitioner can measure number of heartbeats per minute (rate), assess if pulse is regular or not (rhythm) and identify strength (volume) of pulse.
| Normal range of resting pulses | |
|---|---|
| Age | Beats per minute (BPM) |
| Babies to Age 1 | 100-160 |
| Children ages 1-10 | 60-140 |
| Children age 10 and adults | 60-100 |
| Athletes: | 40-60 |
Common cardiac investigations
We have now reviewed the healthy heart. The next section will describe an overview of some of common investigations for the diagnosis, assessment, or exclusion of cardiac disease. These will follow a full clinical consultation and examination.
| Name of test | What it is | Rationale |
|---|---|---|
| Pulse | Manual measurement of arterial pulse. | To measure number of heartbeats per minute (rate), assess if pulse is regular or not (rhythm) and identify strength (volume) of pulse. |
| Blood pressure (BP) | Recorded as two readings: systolic and diastolic, e.g., 120/80mmHg
|
High blood pressure very rarely has any symptoms. Measuring someone’s blood pressure is the only way to know what it is. ABPM provides a full 24-hour profile of someone’s blood pressure. HBPM can reduce the “white coat effect” and can provide several recordings over a number of days. It also promotes self management. |
| Venous blood tests |
|
To assess general health, risk factors for cardiovascular disease or damage to heart muscle. |
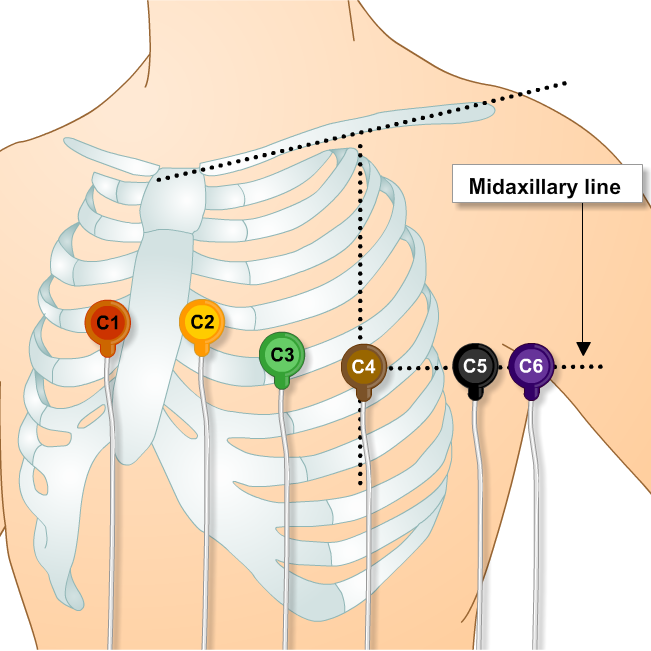
| Electrocardiogram (ECG) | Recording of the electrical signal between electrodes which are placed on chest, wrist and ankles. | Provides a recording of the electrical activity of the heart in the form of a graph. |
| Exercise Tolerance Test (ETT) | Type of ECG which records the electrical activity of the heart when walking and talking on a treadmill and/or bike. | Can be used to diagnose angina and assess its severity. |
| Echocardiogram (‘echo’) | Ultrasound scan of the heart | To assess the size of the heart, how well the heart muscle and the valves are working. |
| Chest x-ray (CXR) | Imaging of the heart, lungs, airways, blood vessels and the bones of the spine and chest. | Useful for showing the size and shape of the heart, detecting chest disorders and showing any fluid in the lungs. |
| Ambulatory ECG / Event recorders | Type of ECG which monitors electrical activity over a period of time as someone goes about their normal activities. Small metal electrodes are attached to the chest. Wires from the electrodes are connected to a small lightweight recorder (Holter monitor). | Used to detect, characterise and record heart arrhythmias. |
Key messages
On completion of this section you should be able to:
- Understand the anatomy and physiology of the normal heart
- Describe the coronary circulatory system
- Describe the conduction system of the normal heart and relate it to the electrocardiogram
- Understand the heart’s relationship to other body systems
Integration of the heart on body systems
The activity of the heart and cardiovascular (CV) system is regulated to ensure adequate blood supply to all tissues and organs throughout the body. There are three main systems involved in the regulation of the CV system: the nervous system, the kidneys and the endocrine system. The rate of the beating heart is normally determined by the pacemaker of the heart i.e. the sino-atrial node. The rate of the pacemaker is modulated by the autonomic nervous system.
Mechanical contraction of the heart
Immediately following the initiation of the electrical activity in the heart, myocardial contraction occurs. This generates the pumping action of the heart.
Electrical activity of the heart
Depolarisation and Repolarisation
The heart cannot pump unless there is electrical stimulus first. As these electrical impulses are initiated from the Sinoatrial node (SA) node and travel in wave form through the heart, a cyclic process of depolarisation and repolarisation occurs. Depolarization is considered to be the active state, and repolarisation is the resting state. During depolarisation and repolarisation, four main electrolytes (sodium, potassium, calcium, and chloride) move across the cardiac cell membrane. These actions are continuous and sequential, and generate the wave form of the ECG. This describes the electrical activity of the heart.
Conduction system of the heart
The pumping action of the healthy heart is triggered by electrical signals sent across the heart muscles. The electrical signal starts in the sino-atrial node, spreading to the atrio-ventricular node and down through the bundle of His to the right and left bundle branches and the purkinje fibres.


