The GP refers Sheila to the Cardiac Rehabilitation team.
Following her referral, Sheila’s case is discussed by the cardiac rehabilitation team. Given her difficulties in attending external appointments, the community cardiac physiotherapist telephones Sheila and arranges to visit her in her home.
For more on Cardiac Rehabilitation see the Cardiac Rehabilitation module.
The physiotherapist reassesses Sheila using the PHQ-9: her score is unchanged from previously. He decides to use a Decisional Balance Box tool to help Sheila to think about the benefits and drawbacks of starting a structured exercise programme.
| Decisional balance | Benefits | Drawbacks |
|---|---|---|
| Change |
|
|
| No Change |
|
|
Referral letter for Sheila
The MooringsHill Street
Heartlough
Re: Sheila Mackay
I wish to refer this lady for cardiac rehabilitation. She has also been referred to the Cardiac Psychology team, for cognitive behavioural therapy.
Age: 76 years
Social: Lives with husband, in rented first floor flat. Daughter visits weekly. No other services.
Presenting complaint: Heart failure with increasing breathlessness. Moderately severe depression.
Past medical history: Heart failure diagnosed four years ago. Previous history of NSTEMI x 2
Mobility: Increasing difficulty mobilising and going upstairs, due to breathlessness.
Medications: Furosemide (80mgs x 2/day); Lisinopril (20mg daily); Simvastatin (40mgs daily); Asprin (20mgs daily); Cipramil (16mgs daily)
Hobbies: Sings in local choir but unable to attend recently.
Yours sincerely
Dr Gillian MacPherson
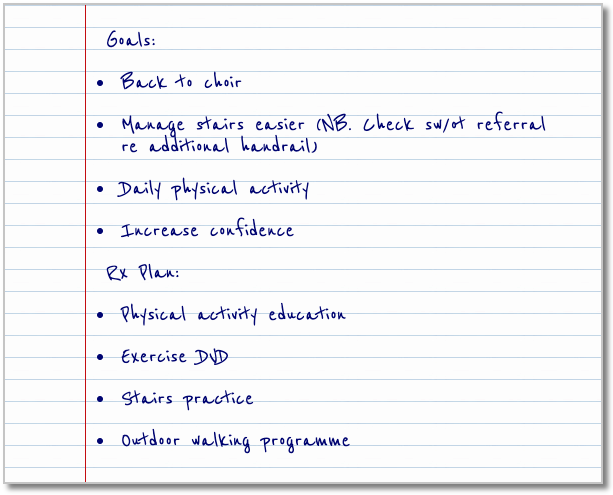
Sheila’s goals
Goals:
- Back to choir
- Manage stairs easier (NB. Check sw/ot referral re additional handrail)
- Daily physical activity
- Increase confidence
Rx Plan:
- Physical activity education
- Exercise DVD
- Stairs practice
- Outdoor walking programme
Pulse point
The mind-body link
In some cardiac conditions, particularly Heart Failure, people experience a reduction in their ability to exercise. This can be due to breathlessness on exertion, fatigue, chest pain or other unpleasant physical sensations. Disuse of muscle can result in a marked reduction in its power and endurance, thought to be as much as 10% loss of strength per week. Consequently, the person’s fitness level reduces and the sensations of fatigue or breathlessness become apparent at a lower level of effort. This can trigger a downward spiral of inactivity causing further weakness and loss of functional ability.
Often this is accompanied by a reduction in the motivation of the person to be active as they prefer to avoid provoking such physical sensations. Often individuals curtail activities in the belief that they will do harm if they become breathless or fatigued, both of which at certain levels, are “normal” reactions to exertion. However, as breathlessness and fatigue are cardinal symptoms of HF, people often feel exercise “brings on” their symptoms and believe it may make their condition worse.
It can be helpful for an individual to recognise and quantify their physical “feelings” whilst being active. This can be done using a perceived exertion scale (Rate of Perceived Exertion (RPE) Scale Cleveland Clinic: Rated Perceived Exertion (RPE) Scale). Once Sheila learns that it is OK to feel “comfortably breathless” and that some aches and fatigue in the working muscles are normal responses to exertion, she become more confident to increase her level of physical activity.
Page last reviewed: 25 Sep 2020


