When the Heart Failure Nurse initially visited Mina to assess her diuretic therapy, Mina indicated that she felt she was losing control of her life and would like to have more say in how her care was organised. When they completed the Distress Thermometer together, it was clear that Mina wanted information and support in a number of areas. The Heart Failure Nurse introduces Mina to the concept of self-management.
Self-management is “a set of approaches with the aim to enable people living with long term conditions to manage their own health and have more control over their health and care”
(Scottish Government, 2008).
The 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure identify key areas where individuals with heart failure, like Mina, might be supported to self manage. PDF link
From their discussion, Mina and the nurse identify specific areas that Mina might be supported to self-manage:
- Pharmacological treatment
- Diet and alcohol
- Exercise
- Sleep and breathlessness
- Psychosocial aspects
Please enable JavaScript in your browser to see this interactive content.
Mina is keen to do what she can independently, in order to manage her conditions.
Mina’s self-management plan
Diet
Fats: Reduction of fat, in particular of saturated fat is one of the pillars of dietary advice to live a healthier life. All individuals with a diagnosis of heart failure should aim to consume less than 2 g of salt per day. Less salt means less fluid retention and this means less work for the heart. Try to keep salt intake less than 2 grams per day. Patients should be encouraged to check the packaging of food to work out the salt content. Other seasoning can help food taste when following a low salt regime.
Often sensible advice is to either:
- Avoid adding salt to food when cooking. Avoid adding salt to food at the table.
- Avoid using salt substitutes such as Lo-salt as this can interfere with your medications.
- Effervescent or fizzy medicines can have a high salt content and should be considered when checking prescriptions.
All patients with heart failure should be encouraged to continue a diet high in fruit and vegetables.
Fluid intake
Some people are advised to limit the amount of fluid they consume in a day. This is something to consider when discussing fluid intake and diuretic therapy in particular. You could also say to Mina that sucking ice cubes or freezing juice can be useful in reducing fluid intake. This should always be discussed on an individual basis and a good way to do this is with the use of a day discussion to determine patients own daily routine.
Fluid restriction to within 2 litres in 24 hours (which includes all foods plus liquids) is part of a self management plan in heart failure. Patients would rather monitor fluid intake to within 2 litres than add in more water pills which make them run to the toilet. As there is no point adding in more diuretics if they then override this by drinking too much liquid which will make fluid overload worse.
Alcohol
All patients with heart failure should be encouraged to remain within the healthy limits for alcohol consumption. A female should not exceed 14 units of alcohol per week and a male should not exceed 21 units per week. This should be spread over the course of a week with at least 2 alcohol free days during this time.
An additional consideration will be the amount of fluid contained in the alcoholic drink e.g. pint of beer.
If patient has a diagnosis of heart failure due to alcoholic dilated cardiomyopathy then they should be strongly advised to abstain.
Weight
Carrying extra fluid causes an increase in body weight. This is why many people are asked to weigh themselves daily and keep a record of it. Weight charts can be found at the back of the CHSS: Living with Heart Failure leaflet.
Patients should be told to weight themselves every morning around the same time without clothes on. Then again of over 2 lbs two days running or 3-4 lbs in a week should be reported to the doctor or nurse. Often this only requires a prescription of a small dose of diuretic for 3 days before reviewing weight gain and symptoms. (often by telephone).
Medication
Mina is on numerous medications due to her multiple conditions. It is the fine-tuning or balance of taking these different drugs that gets the best possible function of the heart. A small adjustment can sometimes make all the difference. Mina may require many different medication considerations in order to reduce her symptoms (NYHA) and keep her symptoms stable. Often symptomatic control is the principal aspect of medications in heart failure management. (Palliation of symptoms) Mina should be advised not to take other non prescribed medications as these can be harmful.
Vaccinations
It is advisable for Mina to have an annual Influenza immunisation and pneumonia immunisation (once only) injection to protect against infection which can place strain on the heart and worsen HF symptoms.
Home Support
Mina is being supported at home with a care package, providing personal care and assistance with cooking for herself and Joe. This should be reviewed regularly to ensure Mina and Joe are receiving the help they need in order to remain at home.
Pulse point
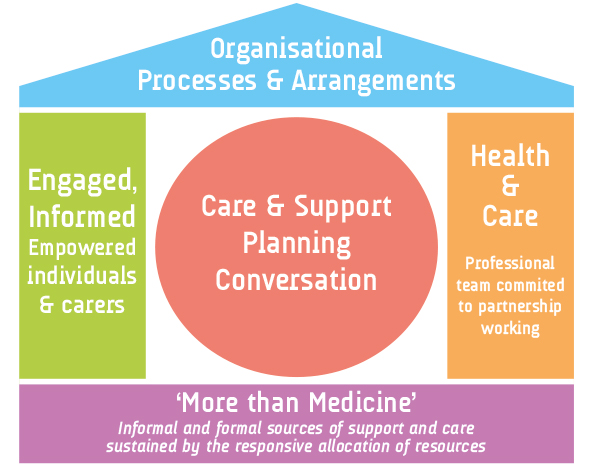
The House of Care approach
“supports and enables people with long term conditions to articulate their own needs and decide on their own priorities, through a process of joint decision making, goal setting and action planning”
(ALLIANCE: Health and Social Care Alliance Scotland (2015).
Page last reviewed: 30 Sep 2020


