Unexpected cardiac arrest in the young is often due to undiagnosed hereditary conditions. Following investigations, Sean is found to be suffering from a hereditary condition known as hypertrophic cardiomyopathy (HCM).
Sean’s parents are, naturally, worried that their younger son may also have the condition and have an OHCA. They are visited on the hospital ward by a genetic counsellor. Genetic counselling is a process by which individuals at risk of a disorder that may be hereditary are informed of the consequences of that disorder, the probability of developing and transmitting it and the ways in which this may be prevented or lessened.
The aims of genetic counselling are to help the individual and family to:
- understand the information about the genetic conditions
- appreciate the inheritance pattern and risk of recurrence
- understand the options available
- make decisions appropriate to their personal and family situation
- make the best possible adjustment to the disorder or risk
Genetic counselling allows information to be made available to “at risk” relatives, promoting early detection and treatment of inherited heart disease in these individuals. It affords the opportunity to address psychological/social/ethical issues which cannot be managed in a routine cardiology clinic.
Pulse point
Genetic counsellors are highly trained, registered healthcare professionals. Further information can be found at:
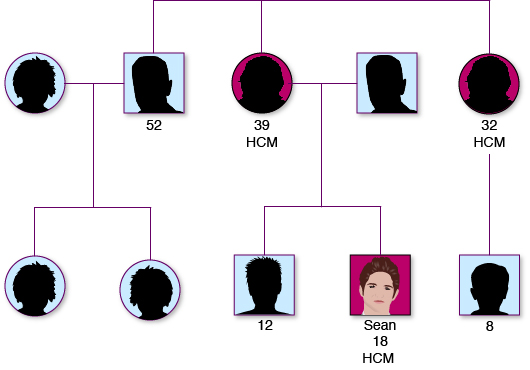
Following counselling, Sean and his family are referred to the cardiac genetic service and offered a clinic appointment to discuss whether they would like to have genetic testing for the mutation that causes Sean’s condition. Sean’s parents decide that they would like to go ahead with this, as they are concerned that his younger brother may also have the gene. Sean is found to have the gene mutation and the family take the decision to offer other family members the opportunity to also be genetically tested.
In Sean’s case, cascade screening of first degree relatives:
- identifies inheritance from the maternal side, therefore, maternal relatives are offered screening
- identifies asymptomatic gene carriers. These are individuals who are genotype positive (so have inherited the HCM gene) but phenotype negative (do not display the physical characteristics of the disease).
- allows risk stratification for SCD to be undertaken and appropriate management offered to those of Sean’s relative deemed to be at risk.
(See Additional Information for best practice guidelines on genetic screening.)
A number of organisations offer support and advice to families in similar situations:
- Network for Inherited Cardiac Conditions Scotland (NICCS, formerly FANS)
- Cardiac Risk in the Young
- Arrhythmia Alliance
Pulse point
Cascade screening:
- Involves targeting close relatives of newly diagnosed patients with inherited cardiac disease, or of a SCD victim, for cardiac and genetic assessment.
- Produces a greater rate of case identification than general population screening.
- Once a diagnosis is confirmed in an individual, testing is extended to first degree and second degree relatives.
- If relatives test positive, their first and second degree relatives are approached and offered testing, and so on.


